Mechanical dyssynchrony, ie nonsynchronous contraction of the wall segments of the left ventricle (intraventricular) or between the left and right ventricles (interventricular), impairs systolic function and ventricular filling, increases wall stress and worsens mitral regurgitation. It is most readily defined by the presence of QRS widening and left bundle branch block (LBBB) configuration on the electrocardiogram. Biventricular pacing by atrial-synchronised pacing of the right ventricle and left ventricle via the coronary sinus to the basal or midventricular left ventricle region accomplishes reverse remodelling of the left ventricle, and this mode of therapy is now recommended by both European and US guidelines. Still, however, the precise indications for implementation of cardiac resynchronisation therapy (CRT) are not established.
The optimum QRS duration, in particular, is a matter of ongoing debate. LBBB and QRS >150 s, female gender and non-ischaemic aetiology are established predictors of response. There was initial evidence that CRT may be beneficial even in mildly symptomatic patients (NYHA I or II) and a QRS >120 ms, especially in presence of LBBB morphology.1–3 However, we know now that a QRS duration <120 ms (LESSER-EARTH trial),4 or even <130 ms (EchoCRT),5 may be detrimental. In patients with mild heart failure, CRT defibrillators (CRT-D) may also be beneficial in non-LBBB patients with PR interval prolongation and left ventricular ejection fraction (LVEF) <30 %, but with a QRS duration ≥130 ms.6 Patients with QRS >130 ms may also respond to CRT even if LVEF >30 %.7
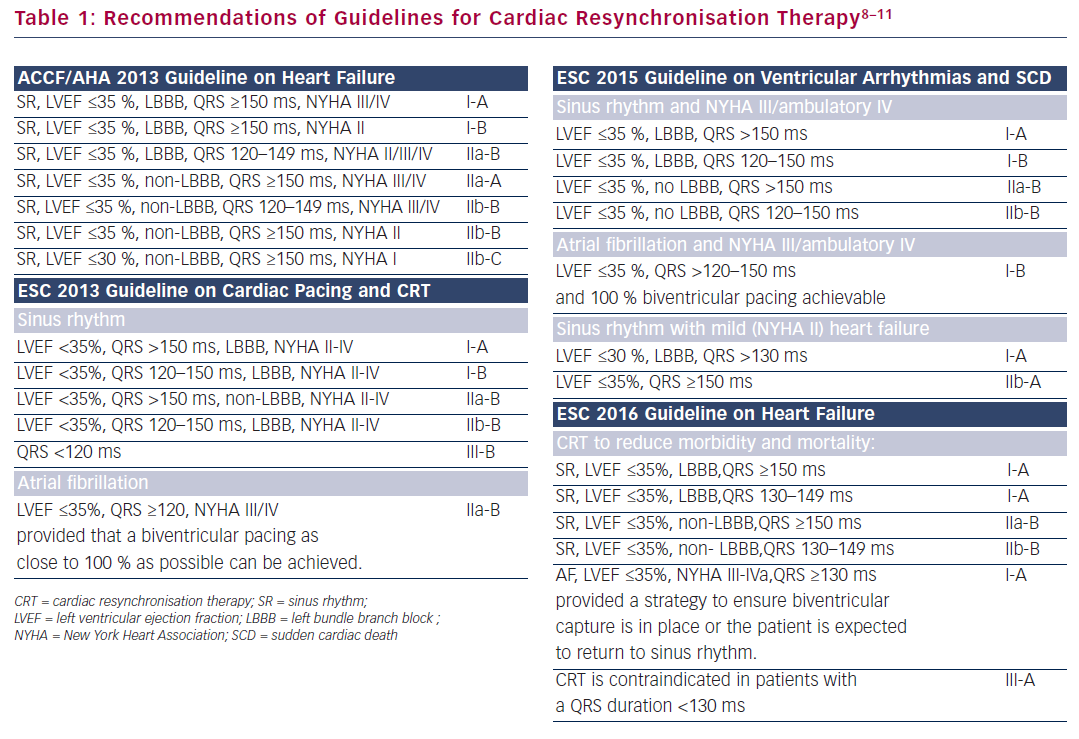
These data are reflected in the recently published ESC guidelines on heart failure.8 In contrast to previous ESC as well as US guidelines,9–11 a minimal QRS duration of 130 ms is now required for recommendation of CRT (Table 1).8–11 Perhaps, this is a reasonable step towards a more rational use of our resources: CRT may be beneficial in certain clinical settings, but as the BLOCK-HF trial has taught us, the potential of increased LV lead-related complications should always be considered.12 CRT is a valuable therapeutic mode, but cautious use is necessary to ensure its continuing efficiency in both medical and socio-economic terms.
Demosthenes Katritsis,
Editor-in-Chief, Arrhythmia & Electrophysiology Review
Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, US