Prevalence of Functional Mitral Regurgitation in Patients with Chronic Heart Failure
Secondary or functional mitral regurgitation (FMR) is a common problem in patients with chronic heart failure (HF) due to dilated cardiomyopathy, regardless of aetiology.1 FMR results from an imbalance between the closing and the tethering forces that act on the mitral valve leaflets.2,3
A chart review of Koelling et al. found that almost half of their 1,436 patients with left ventricular (LV) systolic dysfunction and an ejection fraction ≤35 % also had mitral regurgitation (MR), with 29.7 % having moderate and 18.9 % having severe MR.4 Overall, the prevalence of severe MR in patients with HF and ventricular dysfunction is estimated at nearly 30 %.2 MR confers a worsening of prognosis of patients with ventricular dysfunction.4
Prevalence of Left Bundle Branch Block in Patients with Chronic Heart Failure
Disturbance of (systolic) cardiac synchrony is another problem frequently found in patients with HF. Caused by the cardiomyopathy itself; it further aggravates systolic dysfunction, resulting in an even lower left ventricular ejection fraction (LVEF) and development or worsening of clinical symptoms. The dyssynchrony can either be seen on echocardiography or in a 12-lead electrocardiogram as an intraventricular conduction delay (IVCD) or a bundle branch block.
However, the prevalence of left bundle branch block (LBBB) is low in the general population – about one-third of patients with chronic HF show LBBB with a QRS duration ≥120 ms.5–8 In the EuroHeart Failure Survey, 41 % of all patients with LV dysfunction (LVEF ≤35 %) had a documented QRS duration ≥120 ms. These prolonged QRS durations were due to LBBB or other forms of IVCD in 34 % and due to right bundle branch block (RBBB) in 7 % of all cases.9 Correspondingly, of the 1,391 patients enlisted in the Italian Network of Congestive Heart Failure registry, 6 % had complete RBBB and 31 % had complete LBBB or unspecific IVCD. The annual incidence of LBBB is estimated at 10 % in ambulatory patients with chronic HF and LV systolic dysfunction.10
Concomitant Presence of Functional Mitral Regurgitation and Cardiac Resynchronisation Therapy Indication
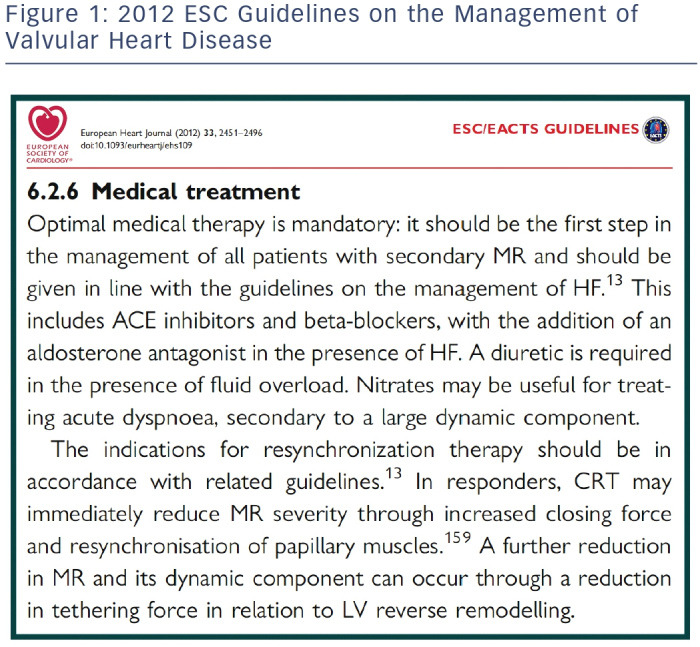
Approximately one-third of patients with an indication for cardiac resynchronisation therapy (CRT) also have moderate-to-severe FMR.11,12 This concomitant presence creates a certain predicament since the FMR may either be a consequence of systolic dysfunction, changed ventricular geometry and size of the left ventricle or it may occur due to this very dyssynchrony.12 In addition, MR itself is known to cause HF progression, as permanent volume overload (produced by MR) has been shown to perpetuate and worsen mechanisms leading to its genesis13 – or as Carabello wrote, “MR begets MR”.14 Physicians are then confronted with two possible therapeutic options – treat the severe MR or resynchronise the ventricles? The European Society of Cardiology (ESC) Guidelines clearly suggest CRT, as it is included in the definition of ‘optimal medical therapy’, which is fundamental for every invasive procedure (see Figure 1).
Cardiac Resynchronisation Therapy as a Valuable Option – Its Indications
CRT resynchronises the contractions of right and left ventricles, and reduces the degree of (systolic and diastolic) FMR both acutely15–18 and in the long term,19–23 at rest and during exercise.24,25 Therefore, CRT is an accepted Class I indication for selected patients.26,27 Although various ways of selecting patients for biventricular pacing have been suggested, the major selection criterion for entry into clinical trials has been the QRS duration. It remains the cornerstone of dyssynchrony assessment, as reflected in the 2013 ESC Guidelines on cardiac pacing and CRT.28,29 These guidelines state that CRT can be considered in patients with chronic HF and left ventricular systolic dysfunction (LVEF ≤35 %) and a documented QRS duration ≥120 ms who remain in New York Heart Association (NYHA) functional class II or worse, despite appropriate medical treatment. CRT is recommended in the aforementioned patient population and LBBB with QRS duration ≥150 ms (Class IA) and LBBB with QRS duration ≥120 ms (Class IB).29
The 2013 European Society of Cardiology Guidelines
CRT aims to normalise intraventricular, interventricular and atrioventricular asynchrony, which may then entail a reduction in left ventricular end-systolic diameter (LVESD) and volume, an increase in LVEF, improvement of the myocardial performance index and a reduction in the diastolic and systolic indices of sphericity.30 CRT further increases longitudinal systolic function by particularly reducing left intraventricular dyssynchrony,31 contributing to the reduction in annular dilation.32 Thus, both directly reducing FMR (surgically or percutaneously) and correcting cardiac dyssynchrony are viable therapeutic approaches in selected patients with symptomatic HF. According to the 2012 ESC Guidelines for valvular heart disease, the percutaneous MitraClip® procedure “may be considered in patients with symptomatic severe secondary MR despite optimal medical therapy (including CRT if indicated), who fulfill the echo criteria of eligibility, are judged inoperable or at high surgical risk by a team of cardiologists and cardiac surgeons, and who have a life expectancy greater than 1 year (recommendation class IIb, level of evidence C)”.33
Responders and Non-responders to Cardiac Resynchronisation Therapy
As is often the case in medicine, some patients do respond to therapy and some do not, despite best efforts. With respect to CRT, Reuter et al.34 defined as non-responders: patients without improvement in NYHA functional class or quality of life score after CRT. The presence of MR grade 0–I was an independent predictor of lack of response. Diaz-Infante et al.35 semi-quantitatively assessed two groups (MR grade 0–II and MR grade III–IV). Patients who died, underwent heart transplantation or did not improve >10 % in their six-minute walk distance, were considered non-responders. MR grade III–IV was a predictor of non-response.13,30,35,36 In patients with FMR, CRT is able to reduce moderate or severe baseline MR to a non-significant grade in one-third of patients. In a study from 2010, CRT reduced MR from significant to non-significant in 34 % of patients but worsened it to severe MR in another 11 %.13 FMR has been reported to persist in about 20–25 % of CRT patients and, in an additional 10–15 %, it may actually worsen after CRT.37 Cabrera- Bueno et al. observed that six months after initiating CRT one-third of patients with severe FMR had improved to non-significant MR, whereas reverse ventricular remodeling, defined as a reduction of at least 10 % in LV end-systolic volume, was achieved in two-thirds of patients (mean relative reduction ± 35 %).30 However, persistence of severe MR is associated with less or no reverse remodeling, worse clinical course and a significantly higher rate of clinical and major arrhythmic events.13,38,39
A change in LV end-diastolic volume after CRT proved to be the most powerful independent predictor of long-term survival. Reduction of end-diastolic volume strongly predicts lower mortality and fewer hospital admissions for HF in the long term.40
The initial presence of FMR is an independent predictor of lack of clinical response to CRT35 and of less reverse remodeling than in patients without FMR at baseline.30 CRT does have the potential to reduce the severity of MR,13,20 but data about the ‘point of no return’ of MR in systolic dysfunction are lacking. Di Biase et al. identified the degree of post-CRT reduction in MR severity at three-month followup (in 794 patients) as an independent predictor of response, strongly correlated with MR reduction at 12 months.11
Clip After Cardiac Resynchronisation Therapy?
As previously discussed, compared with patients in whom CRT reduces MR, the persistence of severe MR after CRT is associated with less reverse remodeling, poor clinical outcome and a significantly higher rate of clinical and major arrhythmic events.13,38,39 Patients undergoing CRT in accordance with the guidelines of the ESC/American Heart Association (AHA)26,27 without signs of significant clinical improvement may be considered candidates for the percutaneous MitraClip procedure.29 The MitraClip (Abbott Vascular, Menlo Park, California, US) has been developed to reduce MR in the beating heart.41 It aims to adapt both mitral valve leaflets (edge-to-edge) by way of a clip, thus dividing one gaping regurgitant orifice into two smaller ones, effectively creating a double-orifice valve. It was the first percutaneous device for MR to be compared with conventional mitral valve surgery in a randomised trial in patients with structural MR (compared with Endovascular Valve Edge-to-Edge Repair [EVEREST II] trial) and fills a therapeutic gap for patients with severe MR who are considered inoperable or at high peri-operative risk.42,43 Among smaller studies, the EVEREST II trial (189 percutaneously treated patients) and the ACCESS-Europe Phase I trial (117 patients) have already proved this catheter-based treatment to be both safe and efficient with respect to total MR reduction, sustained reverse remodeling of the LV with reduction of LVESD, reduced sphericity and increase of LVEF, and finally clinical benefits such as improvement in NYHA functional class, six-minute walk distance and quality of life data.44–46 However, percutaneous repair is associated with a higher necessity of repeat procedures and less improvement in LV dimensions. These divergences were insignificant though in the subset of patients with FMR.47 MitraClip implantation has become an established therapeutic option in patients with significant MR, particularly elderly patients with substantial co-morbidities and ineligibility for surgical repair; it has found its place as a therapeutic option in ESC Guideline recommendations.33,43,44,48,49
The Percutaneous Mitral Valve Repair in Cardiac Resynchronisation Therapy (PERMIT-CARE) feasibility study50 enrolled 51 symptomatic CRT non-responders with predominantly ischaemic cardiomyopathy and moderate-to-severe FMR in 46 % and severe FMR in 54 %; the authors observed that MitraClip therapy achieved a reduction by at least one degree of MR severity almost instantly in most patients. In addition, there were significant reductions in both end-diastolic and end-systolic LV volumes observed at six and 12 months. The considerable improvement in NYHA functional class achieved within the ensuing 3–12 months is proof of significant FMR being one of the major reasons for a lack of response to CRT.50 Despite certain pre- and post-procedural risks, the procedure was judged feasible and safe, taking into account the high morbidity (logistic European System for Cardiac Operative Risk Evaluation [EuroSCORE] 29.7 ± 19.4 %) of a cohort mostly considered ineligible for mitral valve surgery.50 In-line with recent MitraClip studies,44,49 three out of four patients were in NYHA functional class II or better at discharge and 12-month follow-up.50 This clinical improvement strongly correlated with a significant reduction in FMR severity. Less than 20 % of the PERMIT-CARE patients had FMR of grade ≥2 at discharge and in only 10 % did significant FMR persist at one-year follow-up.50 Long-term observations of FMR changes in CRT patients are still lacking.
Clip Before Cardiac Resynchronisation Therapy?
At present, no articles have been published on MitraClip therapy performed before initiating CRT. This may be due to the recommendations of the 2013 ESC Guidelines on the management of valvular heart disease.33
Conclusions
Symptomatic patients with chronic HF due to dilated cardiomyopathy need to be assessed both before and 3–6 months after receiving CRT, in particular with respect to the progression of pre-existing FMR or the development of new FMR. Response to CRT may be assessed by improvement in NYHA functional class and reverse LV remodeling, characterised by reduction in LV volumes and improved systolic and/ or diastolic function within 3–6 months. On the other hand, reliable predictors of failure to respond to CRT are still lacking. The extent of reverse remodeling is still the most important predictor of long-term prognosis.40,50–53
Considering that overall reverse remodeling was observed in the PERMIT-CARE cohort despite FMR grade ≥2 persisting at six months in up to 70 % of patients, this suggests that even a limited reduction in ventricular loading may induce reverse remodeling in CRT non-responders.50 However, evidence is still lacking.
Peri-procedural and overall mortality out to two years appear to be high in the PERMIT-CARE study, with 5.8 % and 20.0 %, respectively;50 but taking into account the patients’ poor pre-operative conditions and the dismal prognosis of non-responders,37 the possible benefits outweigh the risks.
Unfortunately, there are no data allowing a profound answer to the question: which patients with HF and FMR could benefit most from being treated primarily with MitraClip instead of or before CRT? This might be attributable to the 2012 ESC Guidelines on the management of valvular heart disease, which clearly suggest that a percutaneous MitraClip procedure should be considered in non-responders to CRT only. Proper randomised studies to either confirm or weaken the above-mentioned treatment sequence are clearly lacking. Referring to the guidelines, we therefore strongly suggest a clinical trial in HF-patients with both FMR and LBBB to be randomised to either MitraClip procedure or CRT.