The number of invasive electrophysiological procedures is steadily increasing in Western countries, as techniques advance and the age of the population increases. Gender exerts a profound influence on the epidemiology, pathophysiology and clinical presentation of many cardiac rhythm disorders, and all these factors may affect the outcome of invasive electrophysiological procedures. Disturbingly, most of the current evidence-based electrophysiology practices have been derived from studies enrolling predominantly males, and whether the reported outcomes can be safely extrapolated also to females is unclear. This article will summarise the current evidence on gender-related differences that are relevant to outcomes of invasive electrophysiological procedures.
Gender Differences in Outcomes of Radiofrequency Catheter Ablation
Catheter Ablation of Supraventricular Tachycardia
Gender-related differences in epidemiology of supraventricular tachycardias (SVTs) have been reported by several investigators, includinga twofold greater risk of atrioventricular nodal re-entrant tachycardia in females, 1,2 a double incidence of atrioventricular re-entrant tachycardia in males, 3,4 and a higher incidence of focal automatic atrial tachycardias in pre-menopausal females. 5 In the initial assessment of patients with symptoms suggestive of SVT, epidemiological differences between genders might aid the clinical evaluation.
Gender-specific characteristics should also be taken into account when referring patients to diagnostic electrophysiological tests. In females, inducibility of SVTs can change during different phases of the menstrual cycle; 6–9 a dual atrioventricular node physiology can be elicited more frequently during the luteal phase of the menstrual cycle, 6–9 and the increased cardiac sympathetic tone of the ovulatory and luteal phases of the menstrual cycle may facilitate the induction of automatic SVTs. 1 Male gender, on the other side, is a known risk factor for sudden cardiac death in the presence of atrioventricular accessory pathways. 3,10
Radiofrequency catheter ablation has been shown to be equally safe and effective in both genders, although females are typically under-referred to catheter ablation of SVTs. 5,11–14 In a large cohort of 894 patients undergoing catheter ablation of re-entrant SVTs, Dagres et al. reported no gender differences in safety and efficacy of catheter ablation, although females presented to catheter ablation later than males (185 ± 143 versus 157 ± 144 months after onset of symptoms, p<0.001), and after being treated with more antiarrhythmic drugs (1.6 ± 1.2 versus 1.3 ± 1.1, p<0.001). Notably, females were also more symptomatic and with a higher number of SVT episodes per month (p<0.001). 14 The reasons for the under-referral of women to a treatment that is highly safe and effective (such as catheter ablation of SVTs) are unclear, although a sex-related bias in patient referral may play a role.
Catheter Ablation of Atrial Fibrillation
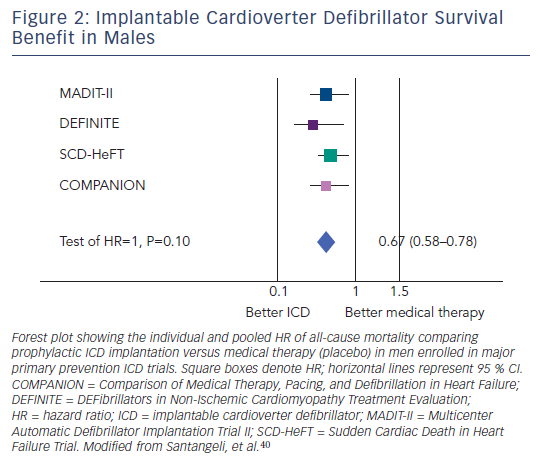
From an epidemiological perspective, the absolute number of women with atrial fibrillation (AF) largely outweighs the number of men, essentially due to a greater longevity of females. 15 Symptoms of AF are more frequent in women, 16 who also experience a worse prognosis with a higher risk of death 17,18 and cardioembolic strokes. 18,19 Surprisingly, women are referred less, and later than men, to catheter ablation of AF. In a multicentre study including 221 patients undergoing pulmonary vein antrum isolation, women constituted less than one-third of patients. Overall, females presented to catheter ablation later than males (median 60 versus 47 months after onset of AF, p=0.04), with evidence of more advanced left atrial remodelling (left atrial diameter of 44.0 ± 6.5 versus 40.6 ± 6.3 mm, p=0.003), and with more co-morbidities. 20 These data suggest the lack of attention towards early clinical signs and treatment in women when compared with men. A possible explanation is that symptoms are more likely to be attributed to stress or anxiety in women than men. In addition, the older age and the higher degree of atrial structural and electrical remodelling disease may in part explain a lower women referral for AF ablation procedures and the gender difference in success rates related to further adverse atrial remodelling in women. In a large series of 3,265 patients undergoing pulmonary vein antrum isolation, Patel et al. found an overall lower referral rate for women, 21 who also presented to ablation procedure older and with more co-morbidities than men. In particular, females had a higher prevalence of long-standing persistent AF (27 versus 20 %, p<0.001), and of non-pulmonary vein sites of firing (50.4 versus 16.3 %, p<0.001), and a lower long-term success rate than males (68.5 versus 77.5 %, p<0.001) (see Figure 1 ). 21
While these findings may be the mere result of a later referral of women to catheter ablation, gender-specific differences in AF pathophysiology may also play a role. In a study on 293 consecutive patients with paroxysmal AF referred for catheter ablation, Lee et al. showed that female gender was an independent predictor of non-pulmonary vein ectopic beats at multivariable analysis. 22 The authors speculated that female hormones might play a role in the higher incidence of superior vena cava ectopic beats in women and that the higher parasympathetic autonomic tone of women 23,24 might account for the higher incidence of superior vena cava site of ectopic beats initiating AF, due to the proximity of autonomic nerves and ganglionated plexi to the superior vena cava. 22 With regard to procedure-related complications, females might experience increased rates of adverse events.
In the large study by Patel et al., women had a higher incidence of haematomas (2.1 versus 0.9 %, p=0.026) and pseudoaneurysms (0.6 versus 0.1 %, p=0.031) than men. 21 Anatomical gender differences due to smaller heart chamber size and pulmonary vein antra in women might affect the ease of performance of ablation procedures, and thus success and complication rate. 14
In conclusion, the overall outcome of catheter ablation in females appears worse than in males, which is likely affected by later referral of females to ablation procedures.
Catheter Ablation of Other Arrhythmias
No significant differences in outcomes of catheter ablation procedures between genders have been reported for atrial flutter. 25 The same is true for catheter ablation of ventricular arrhythmias, although females were largely underrepresented in studies evaluating the role of ablation in the management of ventricular arrhythmias. 26–28
Implantation of Cardiac Devices
Permanent Pacemakers
Females have a lower incidence of atrioventricular block and a higher incidence of sinus node dysfunction. 29,30 As a consequence, this should result in a more frequent choice of dual-chamber pacemakers in females, due to the demonstrated harmful effect of ventricular pacing on the outcome of sinus node dysfunction. 31,32
Surprisingly, in the ‘real-world’, females receive single-chamber devices more frequently. In an analysis on 36,312 elderly Medicare beneficiaries undergoing pacemaker implantation, Lamas et al. showed that male gender was an independent predictor of a dual-chamber pacemaker implantation, 33 thus supporting a sex-bias in pacemaker implantation procedures. 34,35
With regard to complications, females experience more adverse events from pacemaker implantation. 35 Nowak et al. recently reported that women had increased rates of procedure-related complications than men, with higher incidence of pneumothorax (odds ratio (OR) 2.12, 95 % confidence interval (CI) 1.39–3.24), especially when analysing the subclavian vein access group (OR 4.02, 95 % CI 1.91–8.45), and a higher incidence of pocket haematoma (OR 1.49, 95 % CI 1.05–2.11). 35
In addition to women’s older age and co-morbidities, smaller body size of females and a more challenging implantation procedure due to thinner right ventricular wall, smaller blood vessel diameter and a higher prevalence of anatomical variations in venoarterial relationships may explain such findings. 21,35–38 On the other side, female gender seems associated with a better outcome after pacemaker placement, with males experiencing poorer survival following pacemaker implantation. 30,39
In conclusion, despite presenting to pacemaker implantation older, more symptomatic, with more co-morbidities, and experiencing more procedure-related complications, females seem to obtain a greater benefit from pacemaker implantation than males, with a lower long-term mortality.
Implantable Cardioverter Defibrillator
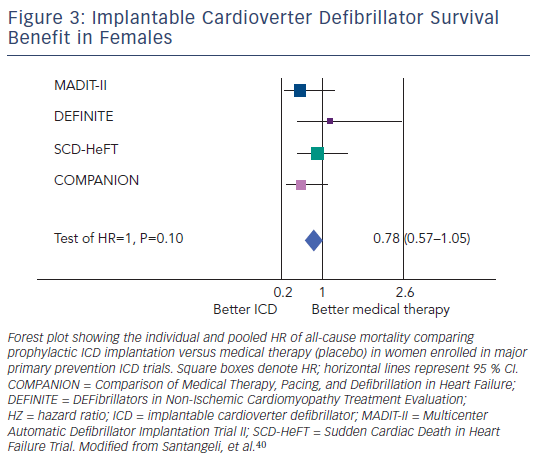
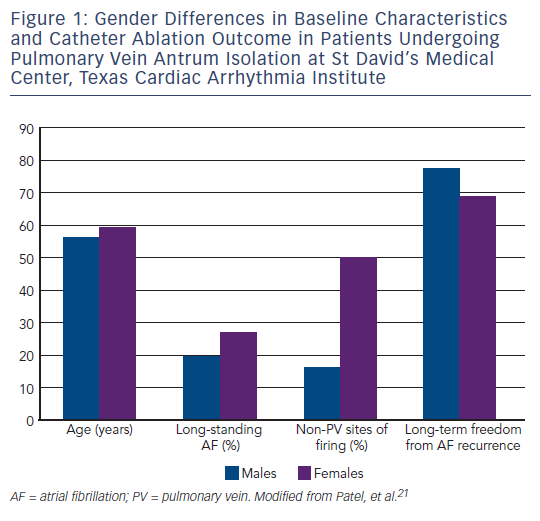
Whether females with severe left ventricular dysfunction earn the same survival benefit as males when treated with prophylactic implantable cardioverter defibrillator (ICD) therapy is still unclear. 40 All studies on this topic have shown inconsistent and conflicting results. 41–44 Subgroup analyses of the Multicenter UnSustained Tachycardia Trial (MUSTT) 43 and of the Multicenter Automatic Defibrillator Implantation Trial II (MADIT-II), 44 reported no significant gender-related difference on the benefit of ICD therapy on mortality. On the other hand, Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) investigators found a significantly lower survival benefit of prophylactic ICD therapy among women. 42 A recent meta-analysis of primary prevention ICD studies (MADIT-II, MUSTT, SCD-HeFT, DEFibrillators in Non-ischemic Cardiomyopathy Treatment Evaluation [DEFINITE] and Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure [COMPANION]) focused on the endpoints of total mortality, appropriate ICD therapies, defined as interventions on sustained ventricular tachycardia (VT) or ventricular fibrillation (VF), and net ICD survival benefit in women compared with men. 45 The pooled analysis included a total of 7,229 patients with severe left ventricular dysfunction (74 % with ischaemic cardiomyopathy). Women constituted 23 % of the total patient population, and suffered from more advanced forms of congestive heart failure and more co-morbidities. Moreover, females received significantly less renin-angiotensin system blockers and coronary revascularisation procedures compared with their male counterparts. Quantitative data synthesis, adjusted for all possible baseline confounders and covariates, showed no significant difference in overall mortality in women compared with men (hazard ratio [HR] 0.96, 95 % CI 0.67–1.39, P=0.84), and significantly fewer appropriate ICD therapies in women (HR 0.63, 95 % CI 0.49–0.82, P<0.001). These data strongly suggest significant gender differences in arrhythmic risk associated with severe left ventricular dysfunction, supporting the concept that sudden cardiac death has a smaller impact on total mortality in women with such disease condition. 45
The presence of gender differences in sudden cardiac death substrates and mechanisms has been reported in several studies. Women are less prone to ventricular arrhythmias except long QT-induced torsade de pointes and drug-induced ventricular arrhythmia, and the incidence of sudden cardiac death is generally lower in women than in men. 46,47 An analysis of the Framingham population revealed that women had a significantly lower incidence of sudden cardiac death in all age groups, with almost two-thirds occurring in subjects without previous diagnoses of coronary artery disease. 47 The lower rate of coronary artery disease in women may contribute to the lower incidence of sudden cardiac death; 48,49 however, differences in susceptibility to ventricular arrhythmia may also play a role. Among patients with coronary artery disease, VT or VF is less inducible in women despite similar ejection fractions, number of diseased coronary arteries and history of myocardial infarction. 50
With regard to outcome after prophylactic ICD implantation, ICD reduced mortality in men significantly (HR 0.67, 95 % CI 0.58–0.78, p<0.001) (see Figure 2 ), whereas in women the mortality reduction did not reach statistical significance (HR 0.78, 95 % CI 0.57–1.05, p=0.1) (see Figure 3 ). 45 In conclusion, available evidence suggests that the presence of severe left ventricular dysfunction may not reliably identify females at risk of sudden cardiac death, and prophylactic ICD therapy based only on left ventricular dysfunction might not be beneficial in this subgroup.
Cardiac Resynchronisation Therapy
Cardiac resynchronisation therapy (CRT) decreases mortality and improves symptoms, quality of life and exercise tolerance in patients with severe left ventricular dysfunction and wide QRS complex. 51–53 Similarly to the ICD trials, women were significantly underrepresented in the CRT trials, being approximately one-third of the total population enrolled. 51,52,54 At variance with ICD studies, subgroup analyses of CRT trials suggest that women may have a better response to CRT, although different studies showed conflicting results. 55–57 In a post hoc analysis of the Multicenter InSync Randomized Clinical Evaluation (MIRACLE) trial, Woo et al. reported significant differences in outcome based on gender, with women randomised to CRT having a significantly lower incidence of the combined endpoint of first heart failure hospitalisation or death compared with women allocated to the placebo arm. On the other hand, no difference was reported among men for the same endpoint. 57 In line with these results, Di Biase et al. found that female gender was an independent predictor of favourable left ventricular reverse remodelling following CRT, analysing data from a prospective registry of 398 consecutive patients (25 % female) undergoing CRT. 58
In the recent Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT), CRT plus ICD was demonstrated superior to ICD alone in reducing the risk of heart failure in a population of patients with dilated cardiomyopathy, a New York Heart Association (NYHA) functional class of I or II, and prolonged QRS duration. 59 Remarkably, a pre-specified sub-analysis confirmed that females treated with CRT plus ICD had a greater reduction in the risk of heart failure than males (HR 0.37 [95 % CI 0.22–0.61] and HR 0.76 [95 % CI 0.59–0.97], respectively, p=0.01 for interaction). 59 In a subsequent analysis, the authors reported that women had consistently greater improvements in reverse cardiac remodelling with cardiac resynchronisation therapy defibrillator (CRT-D) therapy than did men. 60
Several studies have shown gender difference in physiological and pathological remodelling associated with different cardiovascular diseases. 61–63 In addition, in failing human hearts, Guerra et al. demonstrated that the female heart is protected, at least in part, from necrotic and apoptotic death. 64 Based on these observations, it is possible that female patients have a more favourable substrate for reverse remodelling during CRT. 65
On the other hand, Bleeker et al. investigated the gender difference in response to CRT in 173 patients undergoing CRT implantation, 55 and found no significant sex-related difference in the clinical response to CRT. These latter findings were largely confirmatory of what emerged from the largest CArdiac REsynchronization in Heart Failure (CARE- HF) 52 and COMPANION 51 trials, which failed to show significant gender differences in clinical response to CRT.
Conclusions
Gender seems to have a major impact on the outcome of invasive electrophysiological procedures, due to differences in epidemiology and clinical presentation of cardiac arrhythmias, coupled with differences in procedural success and complications. Typically, females with arrhythmias suitable for catheter ablation (e.g. AF and other supraventricular arrhythmias) are referred later to such procedures, which might in part explain the reported differences in outcomes. With regard to implantation of cardiac devices, such as ICD and CRT, the reported gender-related differences in outcomes could be explained by substantial differences in the epidemiology, underlying substrates and clinical course of females with severe left ventricular dysfunction.