Endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardiaca y Electrofisiologia (SOLAECE)
This is an executive summary of the full consensus document on the management of supraventricular tachycardia (SVT) patients published in Europace. The consensus document was prepared by a Task Force from the European Heart Rhythm Association (EHRA) with representation from the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardiaca y Electrofisiologia (SOLAECE). It summarises current developments in the field and provides recommendations for the management of patients with SVT based on the principles of evidence-based medicine, with focus on new advances since the last ESC guidelines.1 It does not cover atrial fibrillation, which is the subject of a separate clinical guideline.
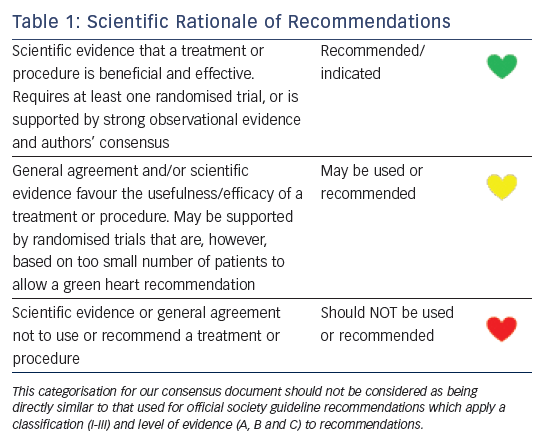
The process for evidence review has been described in the full document. Consensus statements are evidence-based, and derived primarily from published data. Current systems of ranking level of evidence are becoming complicated in a way that their practical utility might be compromised. We have, therefore, opted for an easier and, perhaps, more user-friendly system of ranking that should allow physicians to easily assess current status of evidence and consequent guidance (see Table 1). EHRA grading of consensus statements does not have separate definitions of Level of Evidence.
Diagnosis and Management of SVT
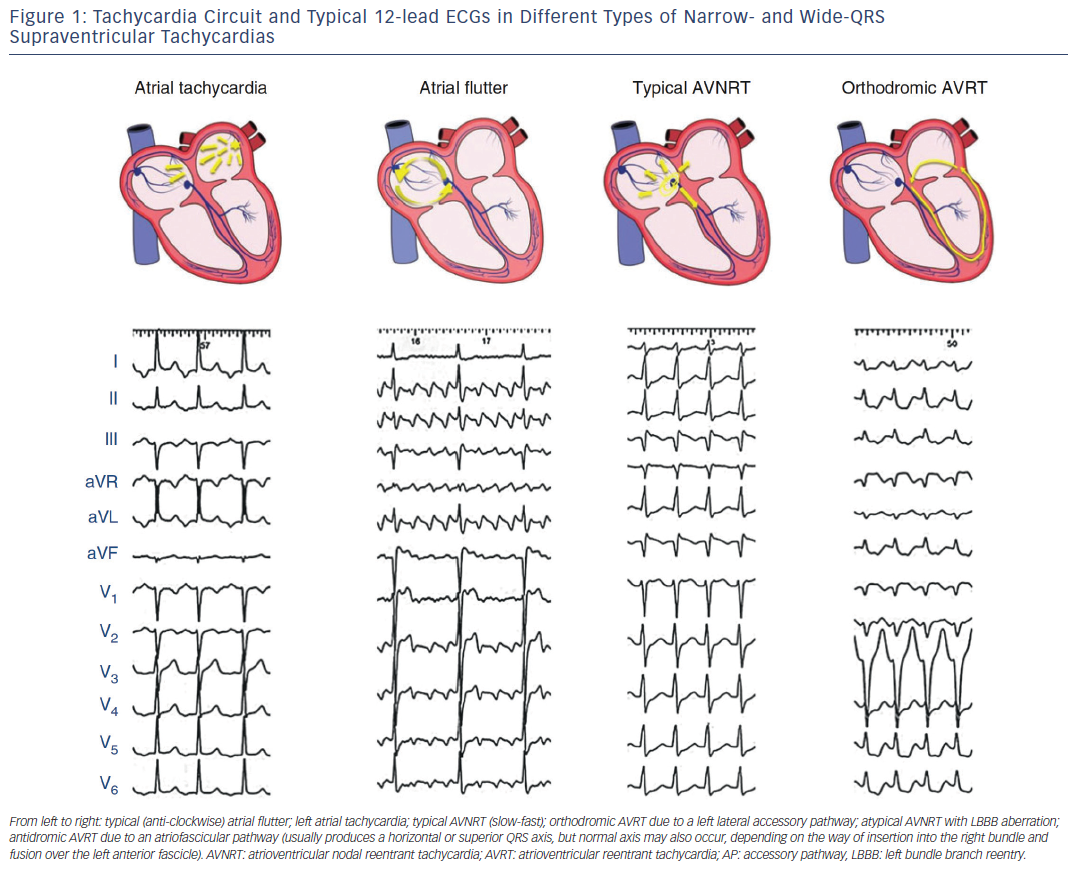
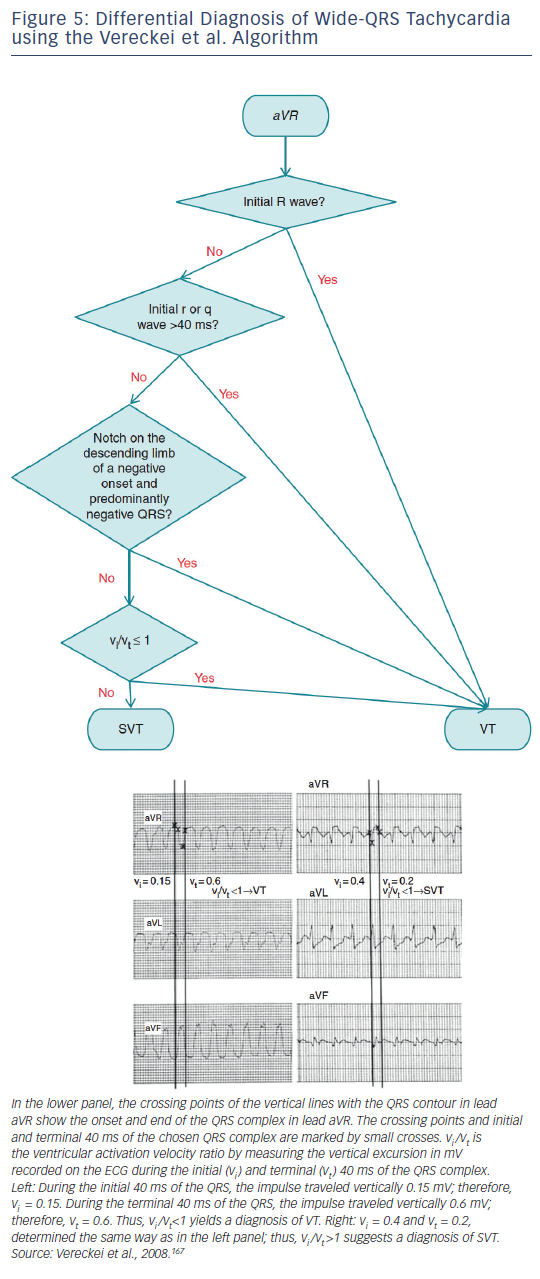
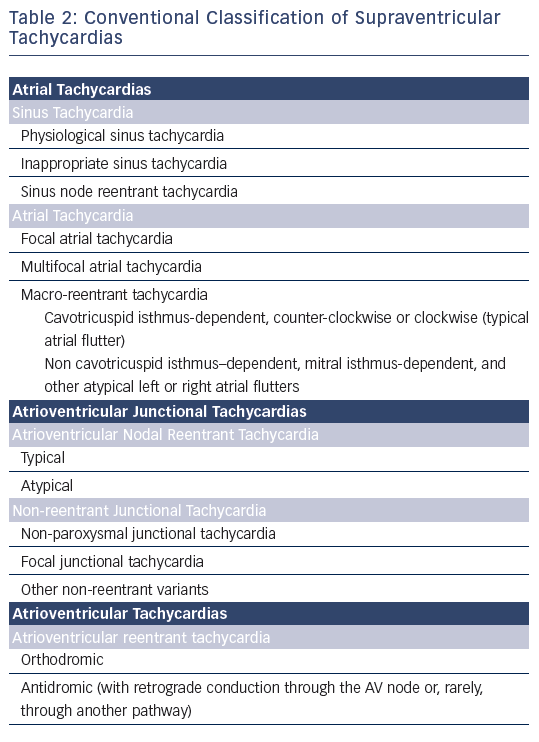
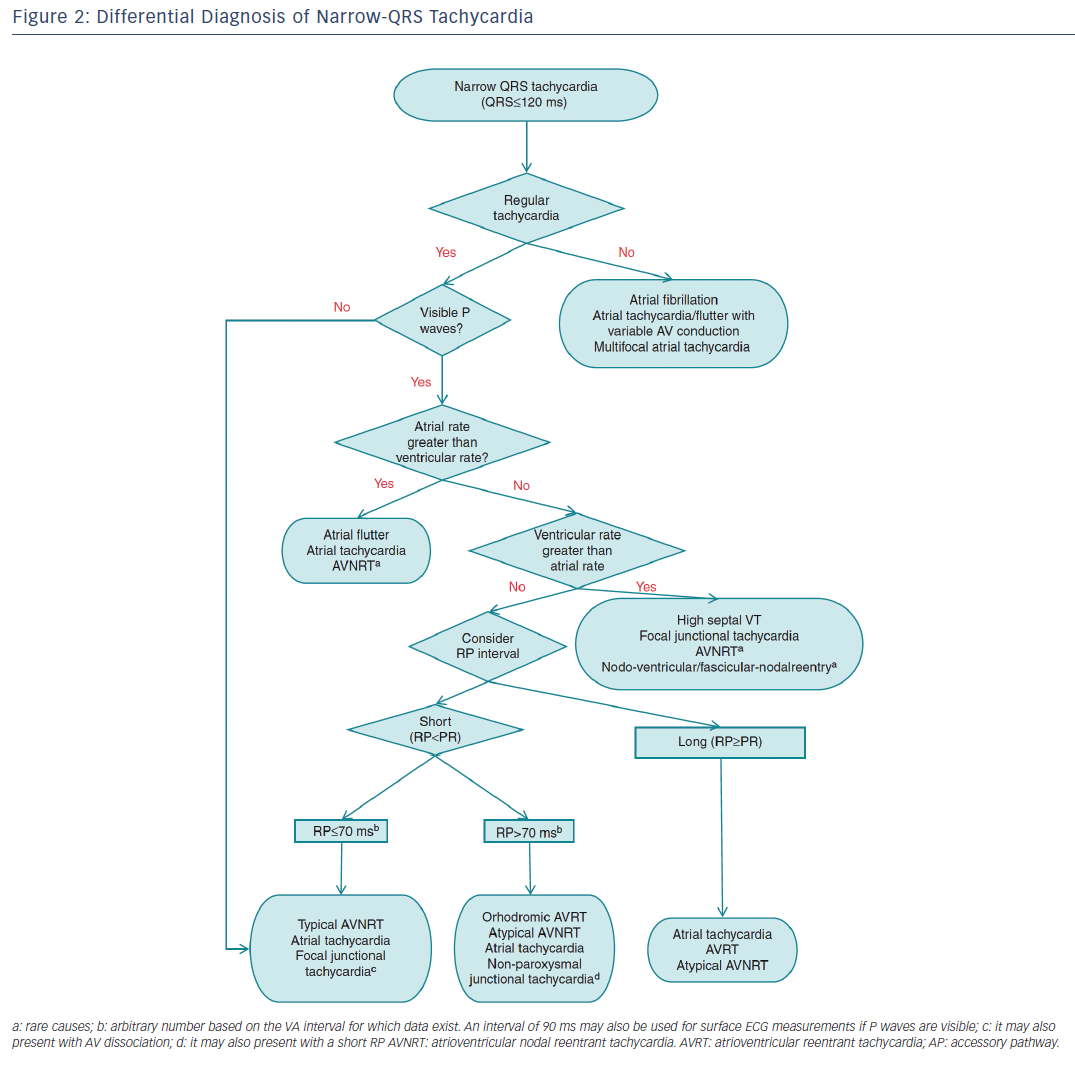
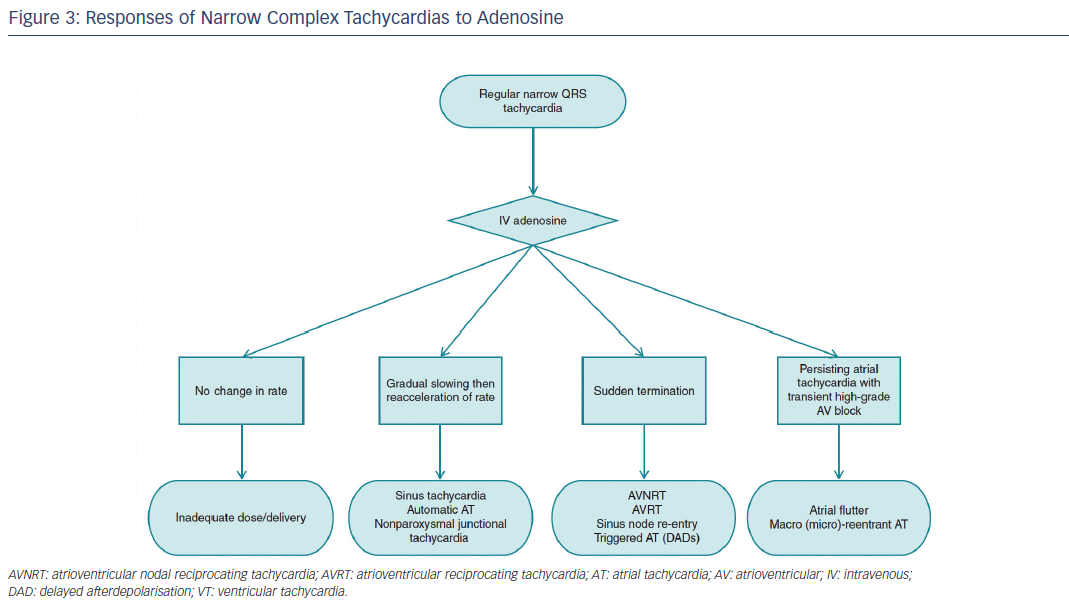
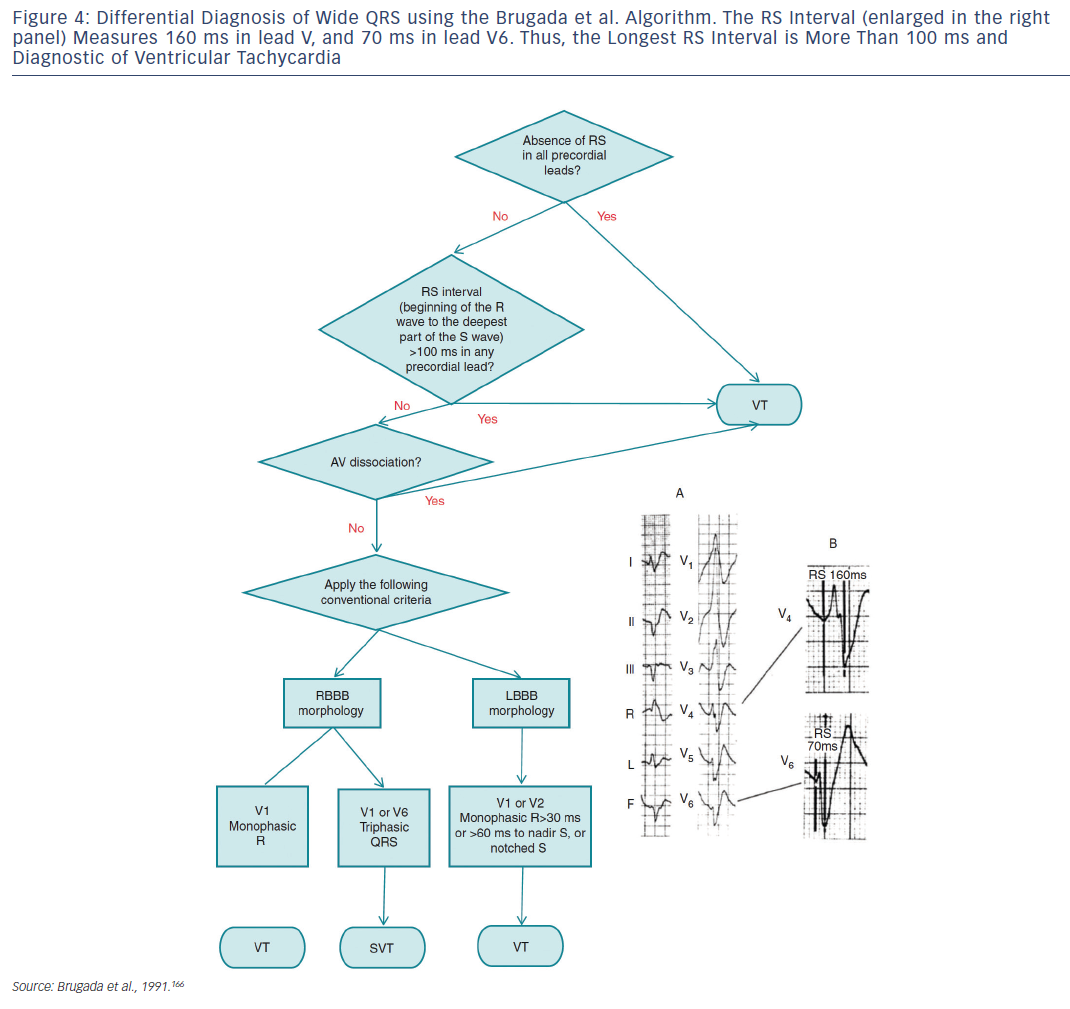
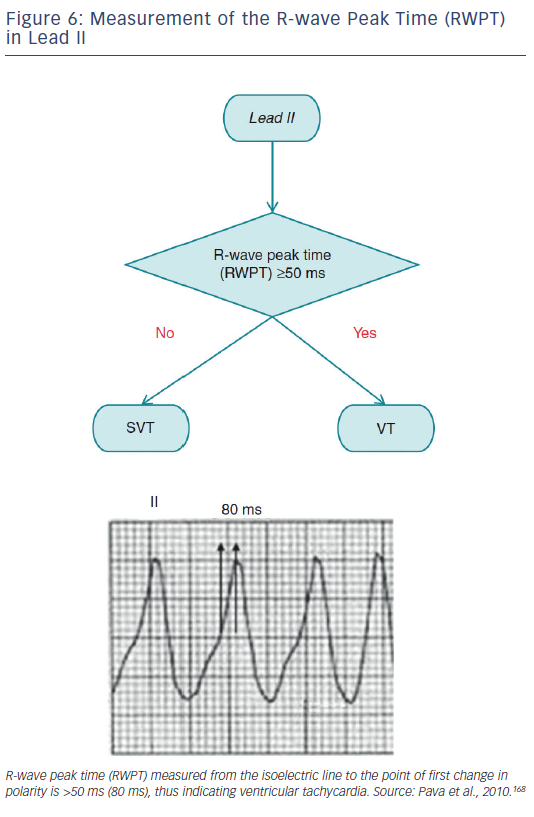
The term supraventricular tachycardia literally indicates tachycardias (atrial and/or ventricular rates >100 bpm at rest), the mechanism of which involves tissue from the His bundle or above (see Table 2). Traditionally, however, SVT has been used to describe all kinds of tachycardias apart from ventricular tachycardias and atrial fibrillation (AF), the mechanisms of which are illustrated in Figure 1. The term narrow-QRS tachycardia indicates those with a QRS duration ≤ 120 ms. A wide-QRS tachycardia refers to one with a QRS duration >120 ms (see Table 3). In clinical practice, SVT may present as narrow- or wide-QRS tachycardias, and most of them usually, although not invariably, manifest as regular rhythms.
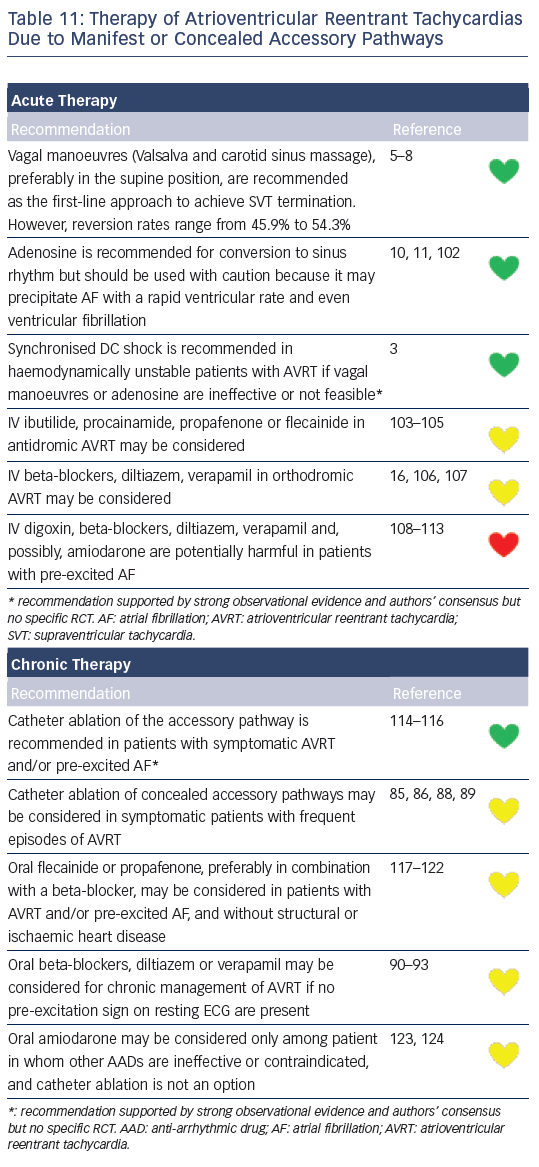
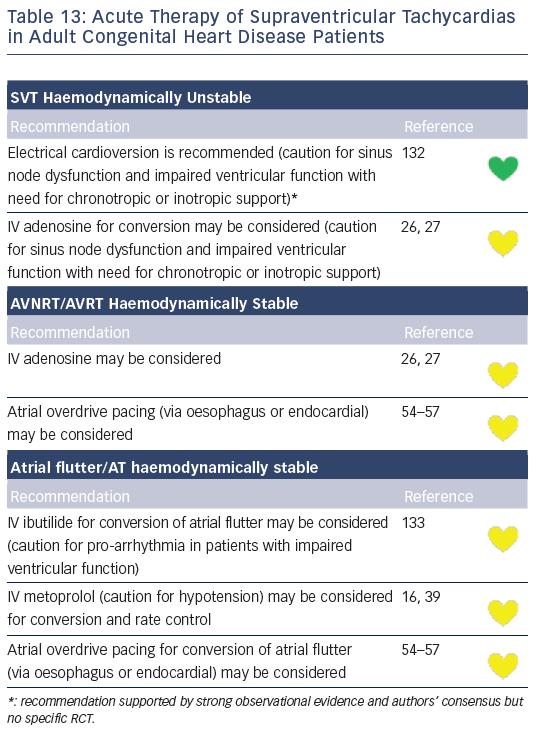
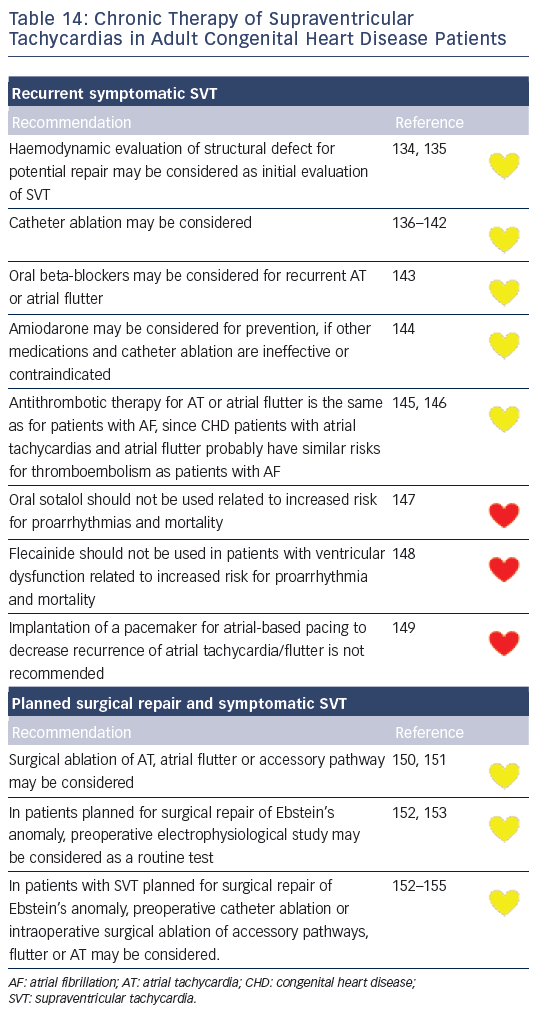
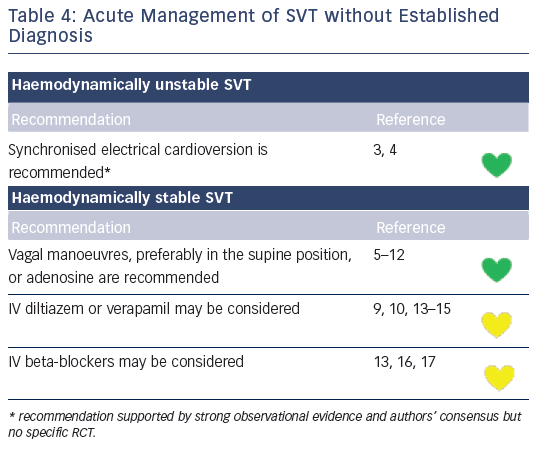
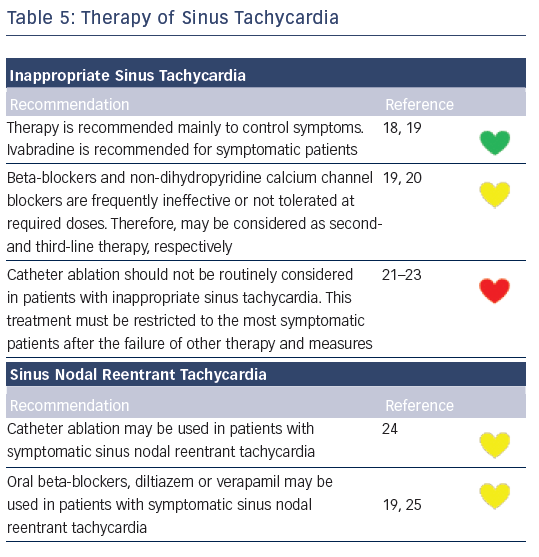
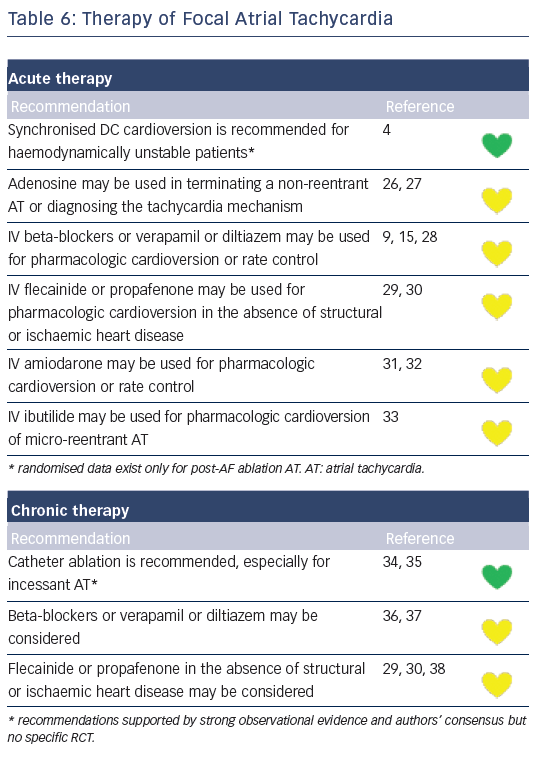
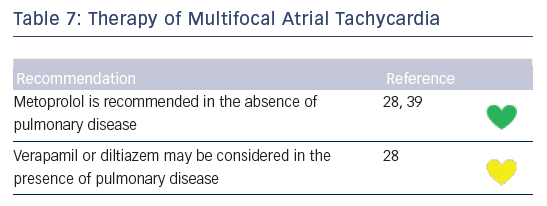
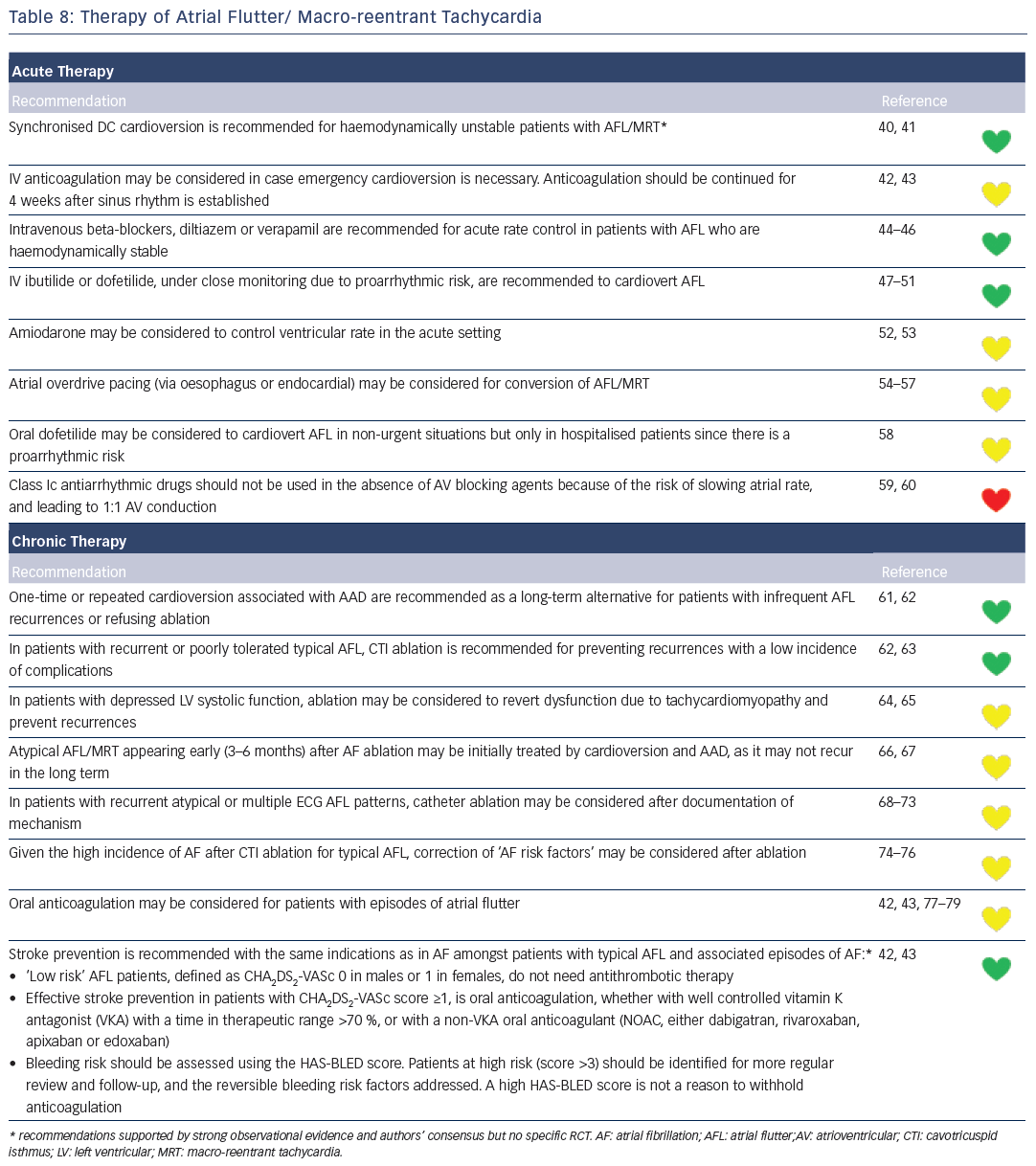
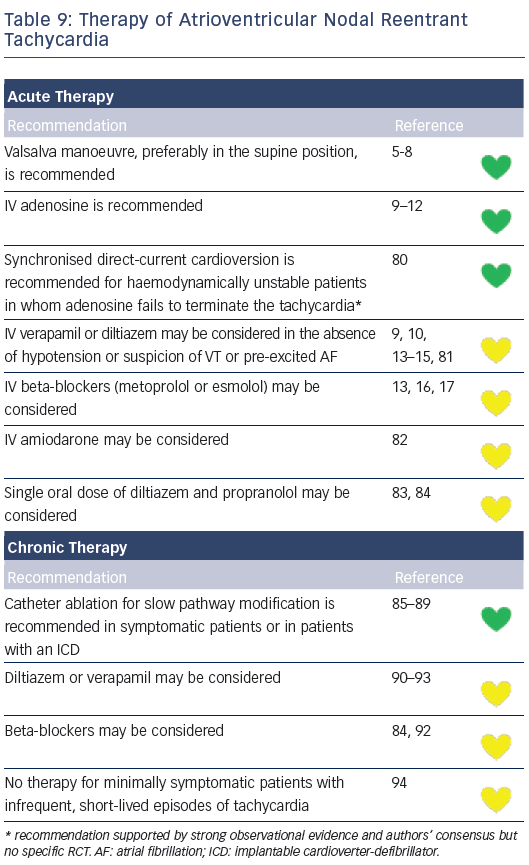
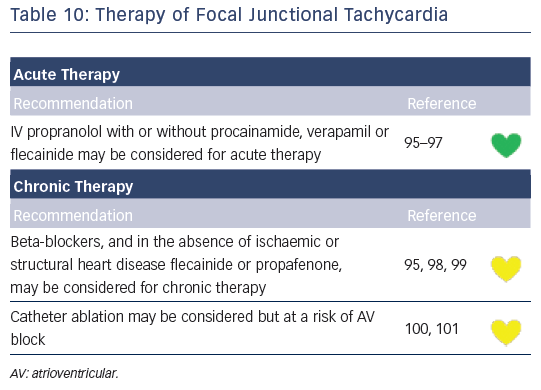
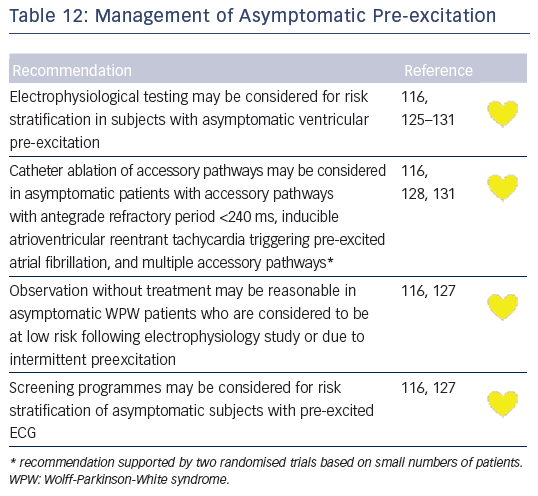
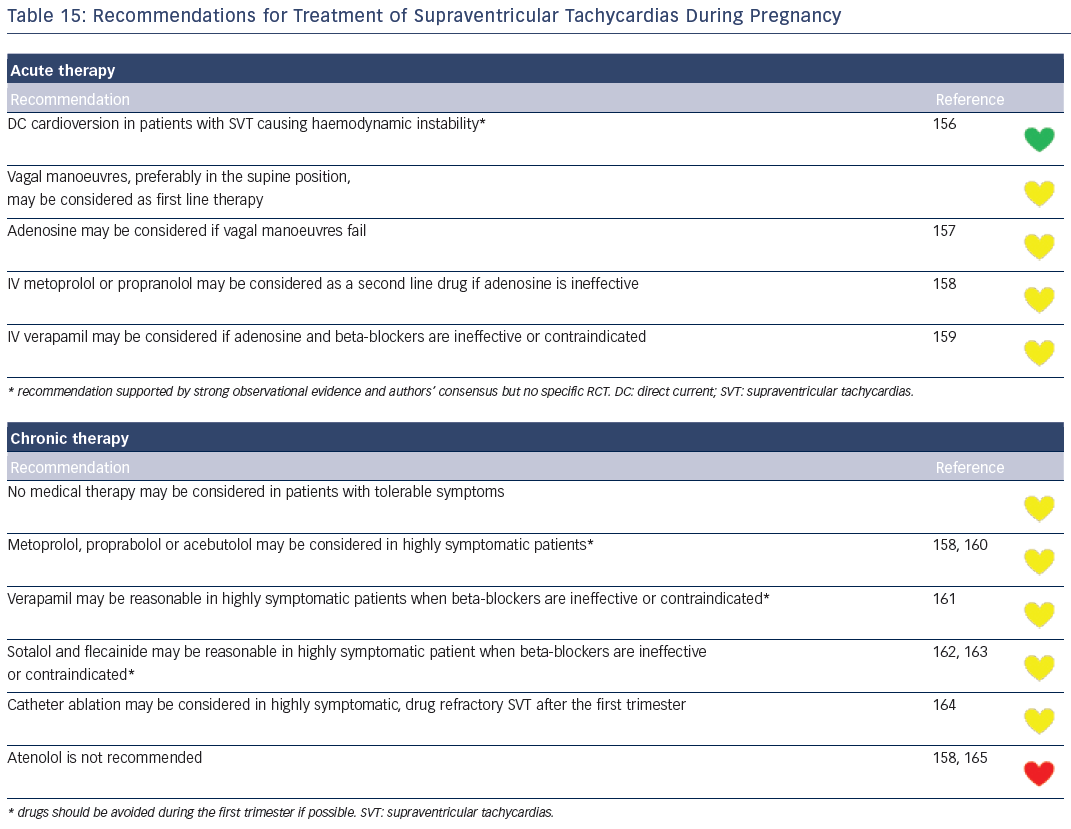
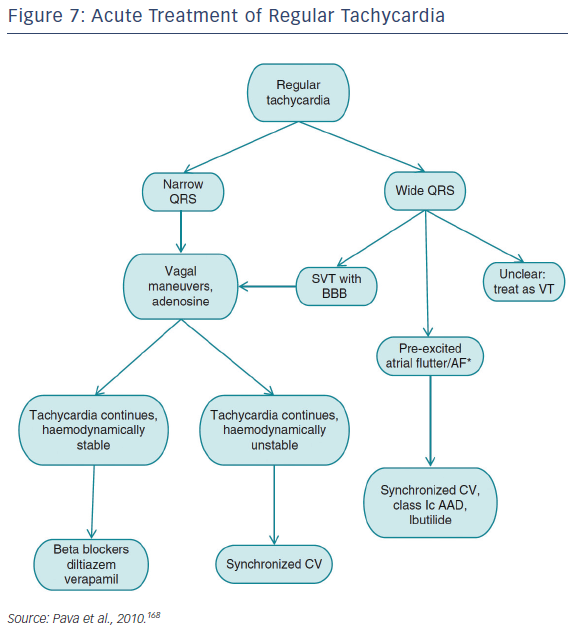
Recommendations for the differential diagnosis of various forms of supraventricular tachycardias, as well as supporting references, are included in Figures 2–6. Recommendations for acute treatment preferences are given. Long-term treatment with antiarrhythmic drugs and/or catheter ablation are also presented and described for each type of SVT, with detailed recommendations given in Figure 7 and Tables 4–15. As compared with the previous SVT guideline from 2003, this consensus document contains several new recommendations based on new trials and meta-analyses, such as the management of patients with asymptomatic Wolff-Parkinson-White syndrome, and the cautious use of certain antiarrhythmic drugs in adult congenital heart diseases. Some discrepancies with the corresponding American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines of 20152 may be related to new evidence that has emerged as well as differences in interpretation of studies and experts’ opinion.