The number of cardiovascular implantable electronic devices (CIEDs) has increased progressively during the past decades, with a parallel increase in the demand for transvenous lead extraction (TLE). Indication and class of recommendation for TLE have been extensively discussed in a recent expert consensus document.1 With the exception of a few prospectively conducted registries,2,3 the vast majority of evidence about the procedural success and complications of TLE has been derived by retrospective analyses of databases, mostly conducted in the USA (Table 1). Few centres in Europe have reported on lead extraction, and objective data are lacking. Furthermore, the majority of past TLE registries have included relatively young patients with few comorbidities. This runs in contrast to the clinical characteristics of patients currently referred for TLE. Improved pharmacological therapy for heart failure and more extensive use of cardiac resynchronisation therapy have resulted in a significant prolongation of patient survival. However, patients with CIEDs are now significantly more frail, present with a greater comorbidity burden and are treated with more complex devices than those implanted two decades ago. The present review discusses the key findings of the European Lead Extraction ConTRolled (ELECTRa) Registry and places them in the context of previous knowledge.
Following publication of the results of a European survey conducted by the European Heart Rhythm Association (EHRA) in 2012,4 the significant underdevelopment of TLE across European countries became clear.
As a consequence, in November 2012, a large multicentre prospective registry of consecutive TLE procedures was initiated by EHRA. This ELECTRa Registry aimed to identify the indication to TLE by various operators and centres, techniques used to perform TLE, and the safety and efficacy of the current clinical practice of TLE in Europe. The results of the registry have been recently published in the European Heart Journal,5 and further discussed at the most recent annual EHRA scientific meeting in Vienna in June 2017. This registry represents a milestone in the knowledge development of modern TLE. Furthermore, the management of the registry by scientific organisations (EHRA and the EURObservational Research Programme by the European Society of Cardiology) is an outstanding model for conducting industryindependent registries and studies.
The ELECTRa Registry included 73 centres from 19 European countries who enrolled 3555 consecutive patients, of whom 3510 underwent TLE. The primary objective was to evaluate the acute and long-term safety of TLE. Secondary objectives were to describe the characteristics of patients, leads, indications, techniques and outcomes. The complication rates in low- and high-volume (30 or more TLE per year) centres were compared.
The first important observation of the ELECTRa Registry was that infections were slightly more frequent than non-infective indications for TLE, the former accounting for approximately 53 % of cases. As recently discussed by Tarakji and colleagues in a review article on patients at risk of infection,6 CIED infection imposes a substantial financial burden resulting from prolonged hospitalisation, long duration of antibiotic therapy, device explanation and eventually re-implantation. Moreover, in the ELECTRa Registry, patients with systemic infection had a near five-fold increase in all-cause mortality compared with the other patient categories. Preliminary analysis of the ELECTRa Registry showed that the 1-year mortality rate was 15.1 % in patients with systemic infection, 6.9 % in patients with a more local infection and 3.0 % in patients without infection. These data confirm the extremely poor prognosis of infected CIED patients, and call for action. Although the ELECTRa Registry has not reported data regarding time delays between diagnosis of infection and TLE, it could be hypothesised that the higher mortality rate observed among patients with CIED infection may result at least in part from a significant delay to definitive treatment. Mortality rates in these situations may be modifiable, with early recognition and prompt treatment. The first presentation of patients with CIED infection is frequently detected by non-electrophysiologists, who usually start treatment with local or oral antibiotics. Thus, the education of emergency department physicians, primary care providers, infection disease specialists and general cardiologists regarding the diagnosis of CIED infection and the need for urgent complete removal of all hardware may reduce the associated mortality risk. The findings of the ELECTRa Registry demonstrate that despite successful TLE, mortality remains high for CIED infection. Although this may include both local and systemic infection, it is certainly higher for systemic infection. Moreover, patients with infected CIED frequently have more severe long-standing comorbidities than other patients undergoing TLE. This highlights the need to reduce the incidence of CIED-related infections, especially in certain patient populations, e.g. renal dialysis patients. Thus, one of the key lessons of the ELECTRa Registry may be that patients with device and lead infections require immediate attention and referral to a centre dealing with TLE.
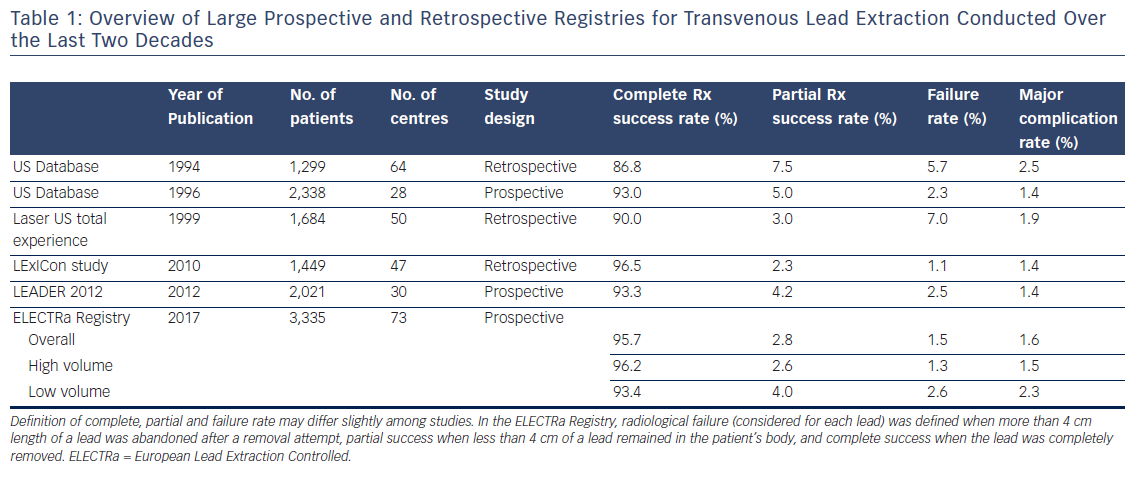
The complete clinical and radiological success rates of TLE were extremely high, approximating 97 and 96 %, respectively (Table 1). This may be a reassuring observation for general practitioners and cardiologists. It is well known that not all indicated patients with CIED-related infection are being referred for lead extraction. A major hurdle explaining this issue is founded on the assumption that TLE is a dangerous procedure, which is contradicted by the findings of the ELECTRa Registry. Indeed, the procedure-related major complication rate (including death) was 1.7 %, with procedure-related death as low as 0.5 %. TLE compares favourably with similar invasive electrophysiological and non-electrophysiological procedures such as catheter ablation, percutaneous coronary intervention and transcatheter aortic valve implantation from a complication risk perspective.
The radiological and clinical success of TLE was higher in high-volume centres than in low-volume centres (Table 1). Moreover, low-volume centres more frequently removed leads with traction alone than did high-volume centres. This point substantiates the need for more adequate training in TLE with sheaths (mechanical, powered or laser) for those operators acting in low-volume centres, which may ultimately lead to an increased removal success rate. As indicated above, the rate of in-hospital procedure-related major complications (the primary endpoint) was 1.7 %, including a mortality rate of 0.5 %, with no significant difference between high- and low-volume centres. However, overall in-hospital major complications were lower in the high-volume centres than in the low-volume centres (2.4 versus 4.1 %). The low-volume centres also showed a double risk of clinical failure of the procedure and of death from all causes during hospital stay. This observation is probably one of the most important key lessons of the ELECTRa Registry.
Although the scope of the registry and the data collection did not allow determination of the minimum number of TLE procedures needed to reduce the complication rate or to increase the survival rate, it may be inferred from the ELECTRa Registry data that the performance of 40–50 TLE procedures per year is sufficient to significantly reduce the likelihood of major events occurring.
The ELECTRa Registry data not only help to identify those factors associated with clinical failure but also, more importantly, with procedure-related major complications. Female gender (OR 2.11), lead dwelling time of more than 10 years (OR 3.54), the use of powered sheaths alone and the femoral approach were all factors associated with higher complication and death rates. A possible explanation for the gender-associated difference in outcome may reside in the fact that women have smaller and more fragile vessels that are more vulnerable to damage. Furthermore, when leads are in situ for a long time, the risk of fibrosis increases, the adhesions become tenacious, the lead is exposed to longer physical and mechanical deterioration that may lead to iatrogenic fracture, and the operator needs to use technologies that require skill and experience to detach adhesions from the vessel wall, thus increasing the risk of laceration and perforation. Therefore, when a low-volume centre encounters a patient presenting with these clinical characteristics, it may be important to consider referring the patient to a high-volume centre.
Another important lesson from the ELECTRa Registry is that in the event of major cardiac complications occurring during or immediately after TLE, patients are often saved if complications are quickly recognised and treated. Although bridge balloons are available and are successfully used clinically, the ELECTRa experience emphasises the need to also have expert surgical back-up available in case of complications. Furthermore, it shows that the outcome of TLE is not solely dependent on the procedure per se. It is also dependent on multiple patient factors and comorbidities that require advanced and highly skilled multidisciplinary team management, including an electrophysiologist, cardiac imaging specialist, microbiologist and surgeon. Such expertise, which allows for coordinated patient management, may be facilitated in high-volume centers.
In conclusion, the ELECTRa Registry findings confirm the previously described observations that the TLE procedure is a safe and effective treatment. It has an acceptable risk–benefit ratio and is comparable with other well-known cardiological invasive procedures. Of course, TLE is accompanied by potential life-threatening complications, the majority of which are manageable by an experienced multidisciplinary team. Multiple factors predict complications, including patient/lead profile, centre experience and procedure volumes, which may suggest caution when accepting a patient for TLE.








