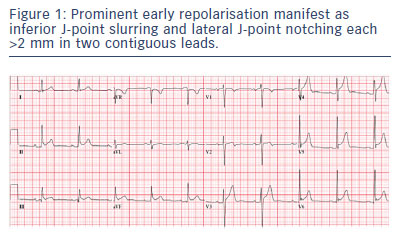
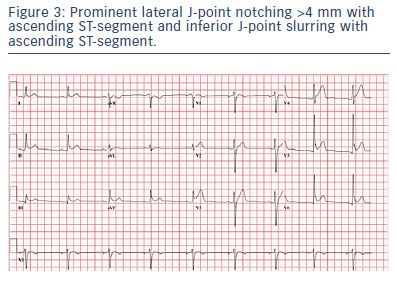
Early repolarisation (ER) is defined as J-point elevation of ≥0.1 mV in two adjacent leads with either a slurred or notched morphology (Figures 1 to 4).1,2 Numerous studies have established an association with ER and increased risk of death and idiopathic ventricular fibrillation (VF).1–5 Clinicians face questions such as patient and family counselling, quantitifying the risk of sudden cardiac death (SCD) associated with ER, inheritance/family screening and therapeutic strategies.
This review emphasises that the arrhythmic risk in most individuals is minimal to none. In others ER may increase the arrhythmic risk of underlying cardiac pathology. Rarely ER syndrome will be diagnosed as a primary arrhythmogenic disorder, with a unique approach to managing associated ventricular arrhythmias.
Prevalence and Arrhythmic Risk
Although the ER pattern on ECG has been reported to have a prevalence of between 1 % and 24 % in cohort studies, idiopathic VF is rare.2,5,6 The incidence of idiopathic VF due to ER in an individual younger than 45 years is estimated to be 3:100,000.4,7 A meta-analysis reporting the incidence of death reported events per 1,000 person- years of arrhythmia, cardiac and all-cause death of 1.68, 4.81 and 17.06 respectively in subjects with the ER pattern during follow-up. The ER pattern was associated with a higher risk for arrhythmia mortality (RR 1.70; 95 % CI [1.19–2.42]; p=0.003) but not cardiac mortality (RR 0.78; 95 % CI [0.27–2.21]; p=0.63) or all-cause mortality (RR 1.06; 95 % CI [0.85–1.31]; p=0.62).6 The data from this meta- analysis also revealed a low to intermediate absolute incidence rate of arrhythmia death (70 cases per 100,000 person-years of follow-up) in subjects with the ER pattern. ER >2.0 mm in the inferior leads was associated with the highest relative risk of 3.02 (95 % CI [1.84–4.96]; p<0.001). Additionally higher amplitude ER (>0.2 mV) in the inferior leads along with the horizontal/descending ST-segment variant, has been reported to have a hazard ratio of arrhythmic death of 3.14 (95 % CI [1.56–6.30]).8 Because the absolute risk remains very low, the incidental identification of the ER pattern should not be interpreted as a high-risk marker. Clinical decisions regarding ER are based on the presence and severity of symptoms and co-morbidities.
The prevalence of ER is higher in athletes, reported to be between 22 % and 44 %,4,8 with the probability of arrhythmic death approximately 0.35:100,000 in competitive athletes.9 Still, the absolute risk remains very low and young, healthy athletes demonstrate an ST-segment morphology associated with ER that does not appear to be associated with an increased arrhythmic risk.8 One study reporting on the clinical significance of ER in 704 athletes (age 25±5 years, ER prevalence of 14 %) reported no cardiac events or ventricular arrhythmias during follow up (mean 6±4 years).10
Clinical Manifestations
ER is most often an incidental benign finding. ER pattern may come to the attention of physicians caring for patients with concurrent cardiac disease. Although ER syndrome may rarely present as syncope,11 limited conflicting data report an association between ER and syncope.1,12
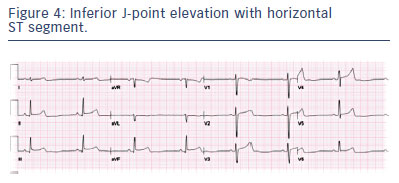
Although a classification system (types 1 to 4) based on arrhythmic risk associated with the spatial distribution of ER has been proposed,13,14 this classification is not universally accepted and has been criticised.15,16 In brief, type 1 ER is found in the lateral precordial leads. It is common among healthy male athletes and is thought to be largely benign. Type 2 ER is found in the inferior or inferolateral leads and is associated with a moderate level of risk. Type 3 ER, noted globally in the inferior, lateral and right precordial leads, appears to be associated with the highest risk.3 Brugada syndrome is classified as type 4, J-wave/point elevation in the right precordial leads. This approach assumes a common mechanistic link between these syndromes, with conflicting evidence to support this hypothesis. The above classification does not take into account the reported ST-segment characteristics associated with risk, with a clear higher risk being associated with the horizontal/ descending pattern.7,8 Additionally, the coexistence of non-type 1 anterior ER (without Brugada changes with and without provocative drug challenge) with inferolateral ER was a key predictor of poor outcome (VF recurrence) in patients with ER syndrome compared with the group with ER syndrome associated with only inferolateral ER.17 The prevalence of the higher risk patterns (e.g. global ER or inferior ER >2 mm with horizontal/descending ST-segment) is substantially lower than the low-risk patterns (lateral ER with ascending ST-segment or inferior ER <2 mm with ascending ST-segment).8,18 The risk has been estimated as low at 1:3,000 even for an adult with ER and horizontal ST-segment.7
Diagnosis of Ventricular Fibrillation due to Early Repolarisation Syndrome
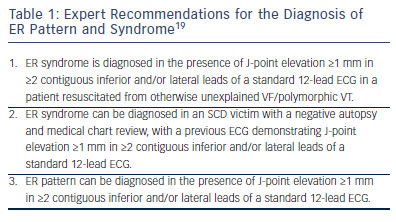
Expert consensus recommendations have been reported for the diagnosis of ER syndrome (Table 1).19
Systematic assessment of survivors of SCD without evidence of infarction or left ventricular dysfunction establishes a causative diagnosis in approximately 50 % of cases.20 A systematic evaluation includes cardiac monitoring, echocardiogram, evaluation of coronary arteries, signal-averaged ECG, exercise testing, cardiac magnetic resonance imaging and intravenous epinephrine and sodium channel blocker challenge. The ER pattern can be intermittent, with 58 % of patients with ER-attributed cardiac arrest having at least one ECG that did not demonstrate the ER pattern during hospitalisation.20
Although genotype data are emerging in case-report fashion, current guidelines do not recommend genetic testing. Even when a familial malignant phenotype is present, genetic testing has not been of assistance.21,22
Prognostic variables of the Early Repolarisation Pattern
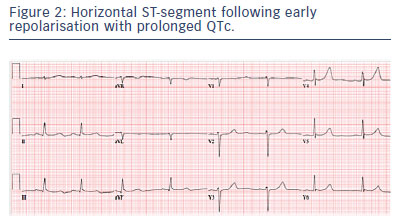
A number of variables have been suggested to modify the arrhythmic risk in ER. However, no risk stratifiers exist that allow for the identification of high-risk individuals who might be candidates for primary treatment. A horizontal/descending ST-segment following ER portends a higher risk in both the general population and in patients with idiopathic VF.2,5 The ST-segment pattern is defined as ascending when there is >0.1 mV elevation of the ST-segment within 100 ms after the J-point and the ST-segment merges gradually with the T wave or as horizontal/descending when the ST-segment elevation is ≤0.1 mV within 100 ms after the J-point and continues as a flat ST-segment until the onset of the T wave (Figure 1, 2, 3 and 4).7,8 Therefore the highest risk occurs with the combination of ER of high amplitude (≥0.2 mV) in the inferior limb leads and a horizontal or descending ST-segment. However the prevalence of the horizontal/descending ST-segment in controls (approximately 3 %) compared with the incidence of idiopathic VF renders this variable still devoid of meaningful clinical utility in the asymptomatic patient.7,8 Additionally, some individuals at risk demonstrate the up-sloping ST-segment pattern.4,7
The incidence of idiopathic VF due to ER with a horizontal ST-segment is estimated to be 0.03 % – 100-fold less than the prevalence.4,7 Thus the absolute risk still remains extraordinarily low. Unless syncope or cardiac arrest are attributed to ER, the mere presence of these ECG features does not warrant intervention per se. Thus, ECG features lack the sensitivity, specificity and predictive accuracy necessary for any clinical utility at present. Although both slurring and notching type ER are observed and may exist in the same patient, the prognostic value of one compared with the other has not been clearly established (Figures 1 and 3).7,20,23
In addition to ECG markers, a number of demographic variables, including gender, family history and ethnicity have been reported to be associated with arrhythmic risk.
A population-based study of central-European descent individuals demonstrated males with ER in the inferior leads had a hazard ratio of 4.32 (p<0.01) compared with the risk in women for cardiac mortality.5 However in a young biracial population (mean age 25, 40 % black) of 5,039 patients followed up for 23 years the presence of ER was not reported to confer an adverse outcome, with age, sex and race almost completely attenuating unadjusted associations of increased total and cardiovascular mortality.24 This study concluded the need for additional studies in patients whose ER pattern is maintained into and beyond middle age.
A positive family history of sudden death has been reported to be significantly more common than in those without ER (16 % vs. 9 %; p=0.17),1 and another study reported a higher prevalence (23 %) of ER in family members of sudden arrhythmic death syndrome probands compared with matched unrelated healthy individuals from the general population (11 % ER).25 Rarely, familial ER has been reported to have an autosomal dominant inheritance pattern with incomplete penetrance. Further studies are required to illuminate inheritance and risk of familial ER.
In a multicentre study of patients with ER syndrome and aborted SCD/ VF involving 81 patients (age 36 ± 13 years, 60 males), inducability of sustained VF during electrophysiology study (22 %) did not predict subsequent arrhythmias followed up (7±4.9 years) by serial implantable cardioverter-defibrillator (ICD) interrogations.27
Although ER is more common in African Americans, there is no clear attributable risk associated with ethnicity and African Americans are not over-represented in idiopathic VF cohorts. In a large population study, lateral or inferior ER in non-African Americans was independently associated with cardiovascular death (HR 1.6; p=0.02), whereas it was not associated with cardiovascular death in African Americans (HR 0.75; p=0.50).26 This study also demonstrated that ER was more common in African Americans (HR 3.1; p<0.01). The hazard of the inferior-only ER could not be estimated because there were no African American deaths in this group. In contrast, in the non-African American cohort, there was a statistically significant association between cardiovascular death and the inferior ER pattern (HR 2.13; p<0.01).
Autonomic Tone
Bradycardia-dependent augmentation of ER is observed in both VF cases and healthy controls. However augmentation of the J-wave and the slope of the regression line (J-point elevation against heart rate) is greater in cases with VF compared with controls (p<0.01).28 Tachycardia, including exercise-testing-related ECG monitoring, tends to show normalisation of the ER pattern. VF often occurs at night when parasympathetic tone is augmented.28 Additionally, the amplitude of ER that may be unnoticeable during daytime in patients with idiopathic VF becomes progressively augmented immediately prior to VF, with bradycardia and an increase in vagal tone.1,29,30 Accentuation of ER due to compensatory pauses after extrasystoles along with the resultant short-long-short sequences may also contribute to VF3.
In a preliminary report involving three French families with an apparent malignant familial ER pattern, the Valsalva manoeuvre was utilised to reveal ‘concealed’ ER.22 However, the relationship between ER manifested by Valsalva and the prognosis is not known.
Early Repolarisation Modifying Risk of Underlying Cardiac Pathology
ER is a much more common modifier of cardiac risk of structural heart disease and primary electrical disorders. ER appears to be associated with an increased vulnerability to ventricular arrhythmias but not to non-arrhythmic cardiac events.31
Patients with J-waves appear to be at an increased risk of ischaemic VF in the event of a myocardial infarction/ischaemia.32,33 In an experimental animal model, the appearance of J-waves following left anterior descending artery occlusion demonstrated modest accuracy (positive predictive value 53 %) for predicting VF during myocardial infarction.34 ER in the inferior leads has also been demonstrated to be associated with increased risk of life-threatening ventricular arrhythmias in patients with chronic coronary artery disease, after adjustment for left ventricular ejection fraction.35 ER in the inferior leads is also reported to predict higher risk of sudden death in non- ischaemic cardiomyopathy patients.36
Limited evidence suggests that the coexistence of ER with a Brugada- pattern ECG is an incremental predictor of arrhythmic events and a more severe phenotype.37–39 Similar observations have been made in long QT syndrome, where major ER was a more potent predictor of symptoms than the QT interval (Figure 2).40 ER has also been demonstrated to be more prevalent in patients with arrhythmogenic right ventricular cardiomyopathy (31 %) compared with the general population, though this retrospective analysis identified no correlation with cardiac events.41 A high prevalence of ER in patients with short QT syndrome has been reported (65 %).42 Given the prevalence of the ER pattern, ER may be viewed as one of many arrhythmogenic factors that is rarely solely responsible for clinical events, but represents a risk ‘cofactor’.
Therapies for Early Repolarisation Syndrome
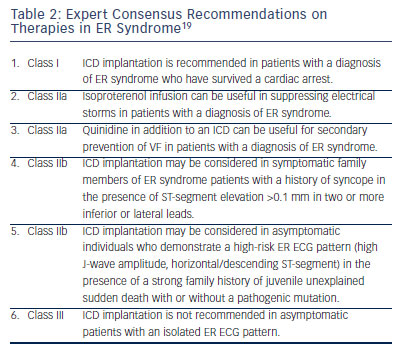
Quinidine is effective for suppression of VF related to ER syndrome, with acute use of isoproterenol in patients who are unstable.43 In this study (n=122; 90 males; mean age 37±12 years), isoproterenol infusion immediately suppressed electrical storms in seven of seven patients. Quinidine decreased recurrent VF from an average of 33 episodes to none over more than two years of follow-up and restored a normal ECG. There was no suggestion of benefit from a number of other anti- arrhythmic drugs (Table 1). An ICD is indicated following cardiac arrest. There is no current risk stratification strategy for asymptomatic patients with ER in the general population and within families with ER (Table 1).
Heritability and Family Screening
ER demonstrates weak heritability in the general population.12,44 Familial ER appears to be transmitted as an autosomal dominant inheritance pattern with incomplete penetrance.25 Familial transmission has also been reported to be more frequent when the mother is affected.44 Potential explanations for unequal transmission include transmission through mitochondrial DNA, effects mediated via sex chromosomes and parental imprinting of autosomal genes. Familial malignant forms of ER syndrome are exceptionally rare.21,22 Asymptomatic individuals with the ER pattern on ECG featuring a mutation considered pathogenic for ER, as well as family members of a patient diagnosed with ER syndrome who present with a diagnostic ECG, may be affected by familial ER syndrome. These families represent a unique cohort, and findings should not be extrapolated to the general population. Unlike these families with a malignant form of familial ER syndrome, the vast majority of familial ER per se is unlikely to portend a substantially increased risk compared with the general population.
Clinical Perspective
- Early repolarisation (ER) syndrome is very rare. Patients with asymptomatic ER and no family history of malignant ER should be reassured that their ECG is a normal variant.
- All patients with the ER pattern should continue to have modifiable cardiac risk factors addressed.
- ER syndrome can be treated acutely with isoproterenol and chronically with ICD implantation and quinidine therapy.
- Family screening and treatment of the asymptomatic individual continues to evolve.
- High-risk family features, including extent of family history of SCD, arrhythmic syncope, and amplitude and morphology of the ER pattern, may lead to consideration of a prophylactic ICD in conjunction with review by an expert centre with a focus on inherited arrhythmias.