Since its first description by Hays in England in 1906, second-degree atrioventricular (AV) block has been a fascinating clinical entity, mainly due to obscure points regarding its diagnosis that emanate from misconceptions and errors regarding its proper definition.1–3 The practicing clinician should be aware of the following points that may assist a proper diagnosis and, consequently, accurate identification of patients in need of a pacemaker.
- Not all blocks are due to conduction system disease. Non-conducted atrial premature beats may mimic AV block. Concealed His bundle or ventricular extrasystoles confined to the specialised conduction system without myocardial depolarisation can also produce electrocardiographic patterns that mimic a type I and/or type II block (pseudo-AV block). Occasionally, retrograde P waves may be present. Thus, AV block due to concealed junctional beats that might represent activity of a pathway inserting into the AV junction may require catheter ablation rather than a pacemaker for therapy.4
- The diagnosis of a type II block cannot be established if the first post-block P wave is followed by a shortened PR interval or is not discernible.
- An apparent narrow QRS type II block may be a type I block with miniscule increments of the PR interval.
- A 2:1 AV block is not necessarily a type II block; it can be nodal or infranodal.2,3 It can be high grade if the sinus rate is low or even a normal response of the AV node to an atrial tachycardia or flutter.
- If the PR is >300 ms, the block is in the AV node. If the PR is <160 ms, the block is in the bundle of His or bundle branches.1
- A pattern resembling a narrow QRS type II block in association with an obvious type I structure in the same recording effectively rules out a type II block, because the coexistence of both types of narrow QRS block is exceedingly rare.
- If the QRS complex demonstrates bundle branch block, the site of conduction can be anywhere in the AV conduction system. If the QRS complex is normal, the block is in the AV node or bundle of His, whereas a type I block with bundle branch block barring acute myocardial infarction is infranodal in 60–70 % of cases.2,3
- If the conduction improves with atropine or exercise, or worsens with carotid sinus massage, the block is in the AV node. If the conduction worsens with atropine or exercise, or improves with carotid sinus massage, the block is in the bundle of His or branches.1
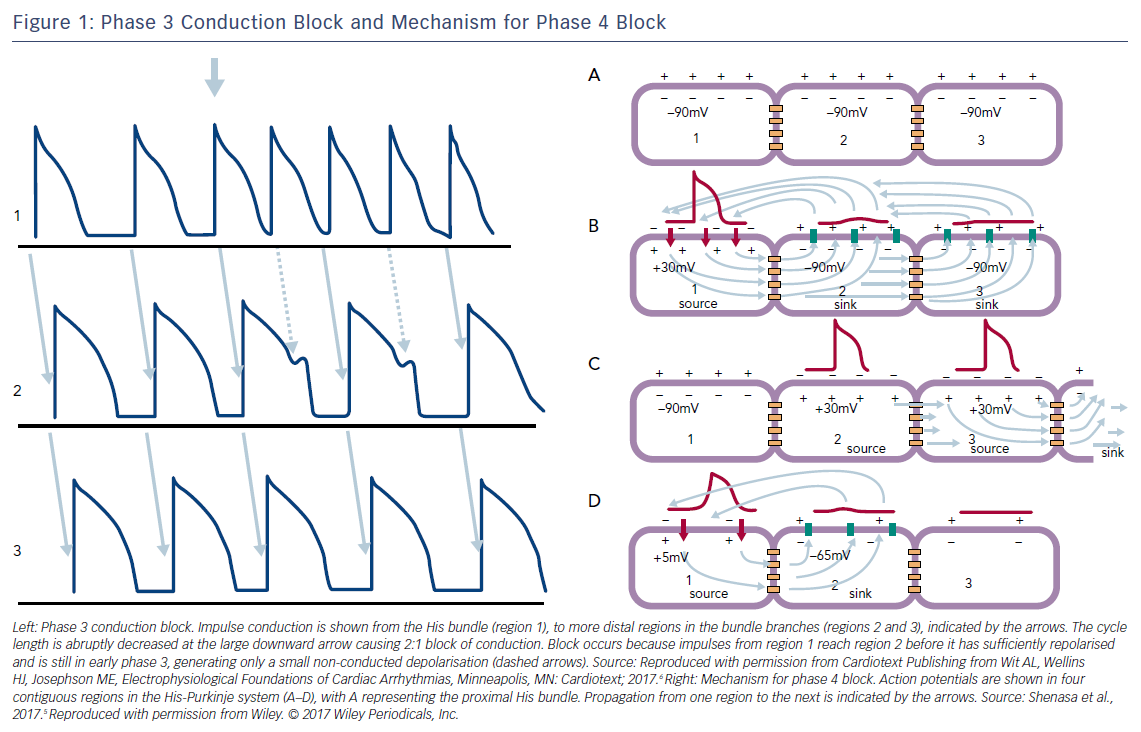
- Although the diagnosis of a type II block is possible with an increasing sinus rate, the absence of sinus slowing is an important criterion of a type II block, because a vagal surge can cause simultaneous sinus slowing and AV nodal block, which can superficially resemble a type II block. Significant PR prolongation before and after a block, and prolonged PP intervals during ventricular asystole are indicative of vagal block that is a benign condition rather than paroxysmal AV block; that is, pause- or bradycardia-dependent phase 4 AV block, which is potentially dangerous for syncope.5 Phase 4 AV block occurs mostly in the diseased His-Purkinje system, when an impulse enters the system during phase 4 diastolic depolarisation (Figure 1).
- Phase 3 AV block, which involves conduction block of early premature impulses in myocardium that is refractory because of phase 3 repolarisation, is a physiological phenomenon that is often due to a high atrial rate (Figure 1). 5,6