Dr Kloppe began his presentation by discussing a 2008 multicentre single-blind crossover study that randomised patients with congestive HF (n=40) either to triventricular (one RV and two LV leads) or biventricular (one RV and one LV lead) stimulation. The primary endpoint was quality of ventricular resynchronisation (Z ratio). The study did not find a significant change in Z ratio but concluded that CRT with triple-site ventricular stimulation was safe and resulted in a significantly higher LVEF and smaller LV end-systolic volume and diameter.24
Since this study, quadripolar leads have been developed. A 2013 study (n=21) compared biventricular and multisite pacing with a quadripolar LV lead. Using an acute pacing protocol, four configurations of multisite and simultaneous RV pacing were tested. In the majority (84 %) of patients, MultiPoint pacing improved LV dP/dt(max) compared with biventricular pacing.25 Only three patients with MultiPoint pacing (one who was a super-responder) experienced no significant additional effect from MultiPoint pacing.
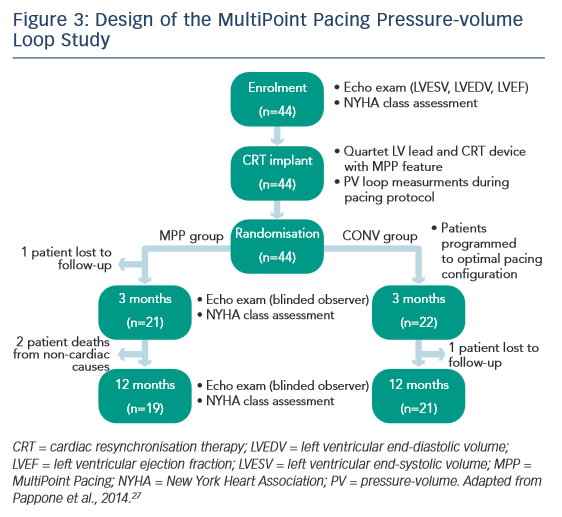
In a prospective multicentre study (n=40), a CRT defibrillator incorporating a quadripolar lead was programmed to deliver MultiPoint pacing with eight different configurations of timing delays. The configuration that yielded the best echocardiographic measurement for each patient was defined as ‘optimal MultiPoint pacing’. The endpoint was analysis of contractility expressed as global radial strain of the opposing walls and stroke volume LV output tract velocity timed intervals (LVOT VTIs). Compared with conventional CRT, the mean peak radial strain was significantly higher for the optimal MultiPoint pacing configuration (18.3 ± 7.4 versus 9.3 ± 5.3 %; p<0.001).26 The median delay between LV1 and LV2 was 55 ms, and between LV2 and RV was 20 ms. In a subanalysis, no difference was seen between ischaemic and nonischaemic patients. The proportion of patients who exhibited improvements in LVOT VTI with at least one MultiPoint pacing intervention over conventional CRT is shown in Figure 2, and suggests that low and non-responders might derive more benefit from MultiPoint pacing.
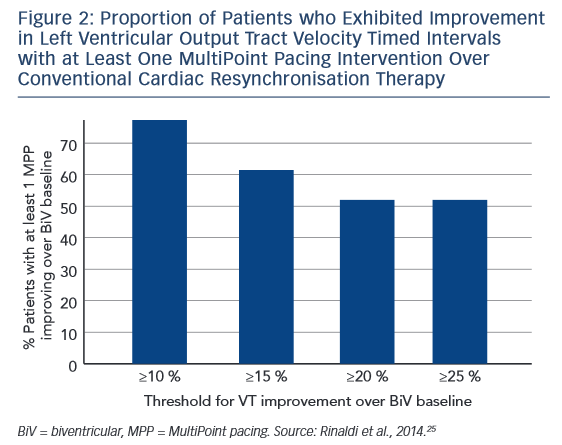
Most recently, a study by Pappone et al. investigated MultiPoint pacing in 44 consecutive patients in an acute setting. Following CRT implantation, consecutive patients (n=44) were randomised to receive biventricular pacing with either conventional LV pacing (CONV) or MultiPoint pacing (see Figure 3). In each case, an optimal pacing configuration was determined based on intra-operative pressure-volume (PV) loop measurements. The primary endpoint was reduction in LV end-systolic volume (LVESV) of ≥15 %. The delay between LV1 and LV2 was 26 ± 15 ms and between LV2 and RV was 10 ± 9 ms. After 3 months, 50 % of CONV patients and 76 % of MultiPoint pacing patients were classified as responders. ESV reduction, EF increase and NYHA class reduction relative to baseline were significantly greater in the MultiPoint pacing group than in the CONV group. In terms of aetiology, non-ischaemic patients had a significant reduction in LVESV compared with ischaemic patients, but no differences were seen in other parameters. A significant increase in MultiPoint pacing group in contractility, stroke volume and EF was seen with MultiPoint pacing. In addition, the best MultiPoint pacing improved acute diastolic function, i.e., change from baseline.27 In 2015, Pappone published 12-month data from this study, showing sustained improvements; these are discussed in the final presentation.28
Another recent study compared biventricular pacing and MultiPoint pacing in a group of 29 patients with a high QRS. The effect of MultiPoint pacing, by means of simultaneous pacing from distal and proximal dipoles, was investigated at any available site, an average of 3.2 pacing sites per patients, and a total of 92 measurements. An increase in LV electrical delay (Q-LV) at any site was seen even with MultiPoint pacing relative to biventricular pacing when taking the best and worst sites. Q-LV was measured at each location, along with the increase in LVdP/ dtmax (maximum rate of rise of LV pressure) obtained by biventricular pacing and MultiPoint pacing. The effect of MultiPoint pacing, by means of simultaneous pacing from distal and proximal dipoles, was investigated at all available sites. Compared with biventricular pacing at any LV site, MultiPoint pacing yielded a small but consistent increase in haemodynamic response. A correlation between the increase in haemodynamics and Q-LV on MultiPoint pacing was observed for all measurements, including those taken at the best and worst sites. The MultiPoint pacing-induced improvement in contractility was associated with significantly greater narrowing of the QRS complex than conventional biventricular pacing. A good correlation was observed between electrical delay and haemodynamic improvement.29
In an ongoing study (n=19), Kloppe et al. measured the acute effect of conventional pacing (SSP) and MultiPoint pacing on dP/dt(max) compared with baseline. A significant increase was observed with MultiPoint pacing relative to SSP but wide inter-patient response to the two interventions was observed. At the recent Heart Rhythm Society meeting, preliminary data were presented from a multicentre prospective study (n=313) that received MultiPoint pacing or biventricular pacing. In the MultiPoint pacing group, EF increased significantly compared with biventricular (42±8 % versus 35 ± 10 %; p<0.001).30
In conclusion, a growing body of clinical data have demonstrated that CRT with MultiPoint pacing can significantly improve acute cardiac contractility and haemodynamic parameters compared with conventional pacing. MultiPoint pacing can further augment the well-described systolic benefits of CRT, likely by better synchronising LV contraction and/or recruiting additional LV myocardial tissue. The MultiPoint pacing-induced improvement in contractility was associated with significantly greater narrowing of the QRS complex than conventional biventricular pacing, However, much remains poorly understood, including the optimal timing of LV1 to LV2 to RV.