Dr Calovic started by examining the percentage of non-responders to CRT. A 2010 evaluation of different studies concluded that agreement is poor among different studies, since different response criteria are used, and concluded that 30 to 50 % of patients do not respond to CRT.31
Strategies for dealing with non-responders include electrogram-based delay optimisation, which is fast, simple and non-invasive, but has not been associated with any benefit in the FREEDOM or SMART-AV trials.32,33 Echo-based delay optimisation is time-consuming, measurements may be inconsistent and its clinical benefit is questionable. Targeting the LV lead to the latest activation has been shown to be effective20 but coronary sinus anatomy may prevent access to the ideal location. The limitations of these strategies have led to the development of MultiPoint pacing LV pacing.
A 2000 study of HF patients with LBBB showed that dual-site pacing gave a greater improvement in systolic function compared with single-site pacing.34 Subsequent studies investigated triple-site pacing24 and concluded that multiple LV pacing sites capture a larger area and reduce dyssynchrony, but involve increased procedure times and increased contrast exposure, as well as lower implant success and the requirement for a Y adaptor or second LV lead connected to the atrial port of the device.
The use of MultiPoint pacing involves a lead with four poles with an ability to pace from three ventricular sites with programmable delays. In a scarred heart, we often see dispersal of the wave fronts of the electrical current. Pacing at two points simultaneously overcomes these obstacles. As previously discussed, numerous studies have demonstrated the acute and mid-term benefits of MultiPoint pacing in improving electrical propagation, acute haemodynamics and dyssynchrony.25–28,35–37 Remaining unanswered questions include: what are the long-term benefits of MultiPoint pacing? Can MultiPoint pacing help patients already receiving CRT?
Determining the optimal pacing vector and inter-ventricular delay can be challenging in conventional CRT. With MultiPoint pacing, the addition of a second LV pulse with another programmable delay gives even more programming options. The MultiPoint pacing loop study evaluated two methods of MultiPoint pacing vector combination selection and multiple delay combinations. In this patient cohort, an empirical method of selecting MultiPoint pacing pacing vectors based on maximising anatomical spacing between LV1 and LV2 cathodes resulted in the best dP/dt response more often than an electrical delay-based selection method. Moreover, pacing with 5 ms LV1–LV2 delay produced the best dP/dt response more often than pacing with 40 ms LV1–LV2.27
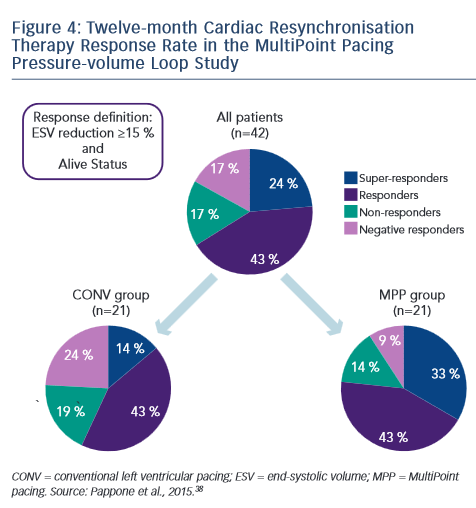
Recently, Pappone published 12-month follow-up data from this study.28,38 The trend observed at 3 months was sustained; LVESV and EF were significantly improved in the MultiPoint pacing group relative to the CONV group. A clinical benefit was also seen: improvement of more than two NYHA classes was seen in a much higher proportion of MultiPoint pacing patients compared with conventional pacing. According to the definition of response (ESV reduction of ≥15 % and alive status at 12 months), 67 % of the overall patient population were responders, with a 76 % responder rate in the MultiPoint pacing group compared with 57 % in the CONV group. This was further subdivided into superresponders (ESV reduction ≥30 %), responders (ESV reduction ≥15 and <30 %), non-responders (ESV reduction ≥0 and <15 %) and negative responders (ESV increase). The MultiPoint pacing group showed a lower rate of negative responders (10 versus 25 %) and a higher rate of super responders (33 versus 14 %) compared with the CONV group (see Figure 4).38 An example of acute haemodynamic measurements and echo measurements were given in a super responder: these included a decrease in EDV from 310 ml at baseline to 235 ml at 3 months and 211 ml at 12 months. The decrease in EF was 35 % at baseline and 41 % at both 3 and 12 months.38
Dr Calovic next posed the question: can MultiPoint pacing improve the response in patients receiving conventional CRT? At CRT implant programmed with simultaneous biventricular pacing, patients were assessed by an echo exam (LVESV, LVEDV, LVEF) as well as undergoing NYHA class assessment. At 12 months, patients underwent follow-up assessments and CRT programming was switched to MultiPoint pacing. Further follow-up assessments were performed at 16 months. Following the switch, the two non-responders to conventional CRT both became responders with MultiPoint pacing while experiencing an additional reduction in ESV of -33 % and -20 % and an improvement in EF of +15 % and +4 % at 16 months relative to the 12-month exam. Five of the six responders to conventional CRT remained responders with MultiPoint pacing, with four patients experiencing additional ESV change of at least -10 %. In terms of NYHA class changes, all patients were Class II pre-implant, all improved to Class II at 12 months and after 4 months of MultiPoint pacing, four patients improved to Class I while the remaining five patients remained in Class II.39
In conclusion, MultiPoint LV pacing in a single coronary sinus branch results in significant improvements in acute haemodynamic function and long-term CRT response relative to conventional biventricular pacing. Non-responders to conventional CRT may benefit from activating MultiPoint pacing and may be converted to responders. In addition, CRT responders may experience additional LV remodeling and/or increased LV function beyond that received from the conventional therapy.








