Catheter ablation has been increasingly used as a treatment for refractory ventricular tachycardia (VT) in patients with non-ischaemic cardiomyopathy (NICM). However, ablation outcomes tend to be quite variable because of the heterogeneity of the aetiology for the NICM and associated VT substrate in these patients.1–3 Patients with NICM can be sub-classified based on specific genotypic and phenotypic findings, including dilated cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy (ARVC), hypertrophic cardiomyopathy, restrictive cardiomyopathy, lamin A/C (LMNA) cardiomyopathy, sarcoid cardiomyopathy, amyloid cardiomyopathy, post-myocarditis cardiomyopathy and left ventricular (LV) non-compaction cardiomyopathy (LVNC).4 While one recent multicentre study reported VT ablation outcomes of all NICM aetiologies, including myocarditis, sarcoidosis and valvular disease,5 most VT ablation studies in NICM have focused on patients with the dilated cardiomyopathy phenotype and exclude patients with ARVC, hypertrophic cardiomyopathy, LVNC, restrictive cardiomyopathy, cardiac sarcoidosis (CS), valvular disease and acute myocarditis.1,6,7
The different NICM aetiologies exhibit discrete substrate patterns. Unlike the distinct dense scar, which exhibits subendocardial to transmural features in patients with prior MI and ischaemic cardiomyopathy (ICM), progression of myocardial fibrosis with predominantly perivalvular and/or intramural/subepicardial patterns is more commonly observed in NICM. This pattern of involvement can be demonstrated on cardiac MRI (CMR), electroanatomical voltage mapping (EAVM) and histology.8–10
Because of the presence of heterogeneous substrate in patients with different types of NICM, cardiac imaging is especially helpful to define the location and extent VT substrate and guide pre-procedural planning. This review will provide a summary of the current understanding of substrate characteristics identified by multimodal imaging and EAVM, the practicality of image integration during ablation procedures, as well as the impact of imaging modality utilisation on VT ablation outcome in various NICM aetiologies.
Value of Pre-procedural Imaging and Image Integration to Guide Refractory VT Ablation in Non-ischaemic Cardiomyopathy
Pre-procedural imaging is helpful to guide VT ablation in patients with healed MI and ICM. In these patients, multimodality imaging can help to identify arrhythmogenic substrate and critical components of VT circuits, leading to decreased radiofrequency ablation time, total procedure time, and improved acute and long-term ablation success rates.11–17 In contrast, the impact of pre-procedural imaging to guide VT ablation in NICM differs based on the underlying NICM aetiology. Pre-procedural imaging can visualise the presence of epicardial substrates and predict when epicardial mapping may be warranted.18–20 Moreover, it localises important structures such as the phrenic nerve and epicardial coronary arteries which can be integrated into the electroanatomical map to avoid complications during ablation.20,21
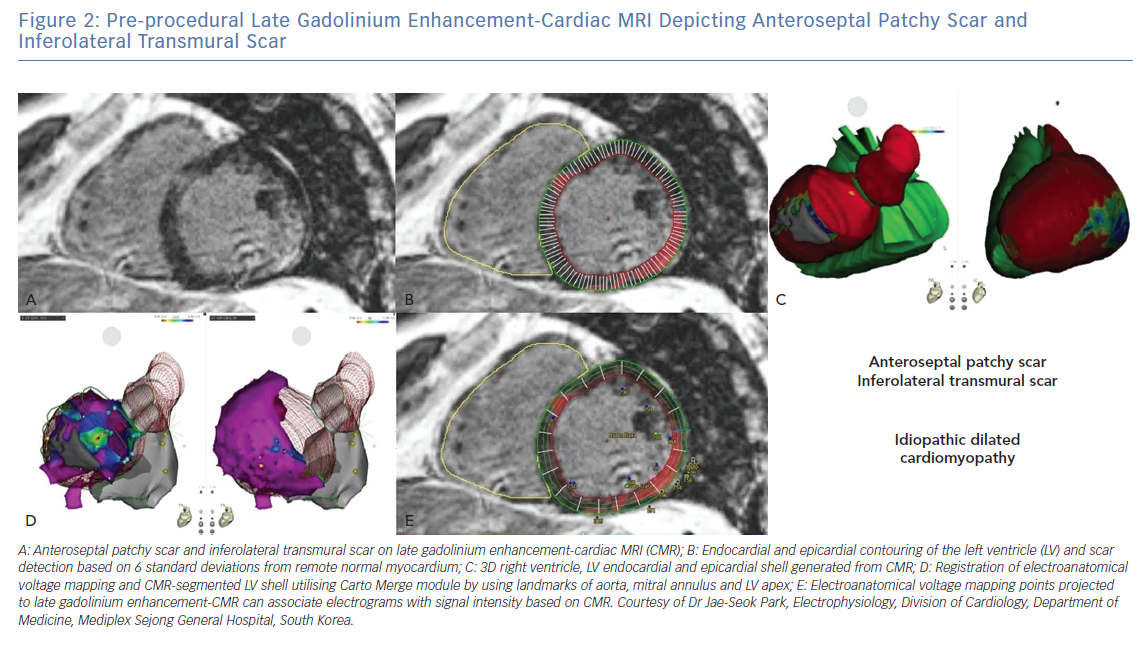
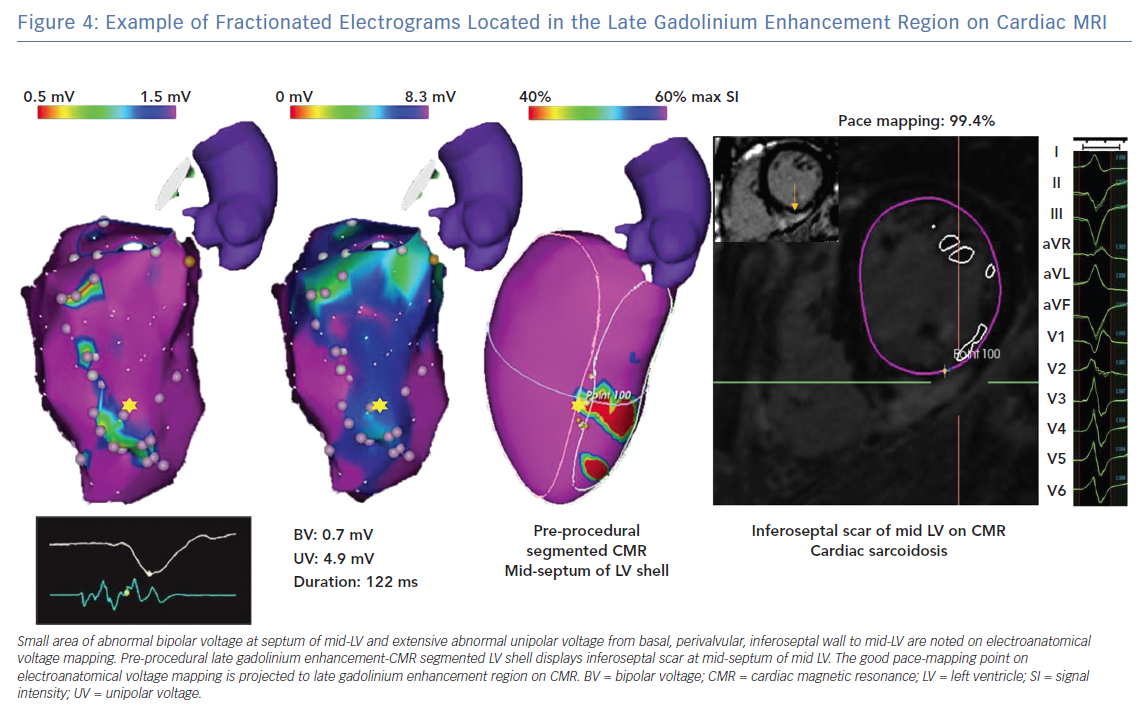
CMR is the most well-studied imaging modality used to guide VT ablation in patients with NICM. Andreu et al. showed no difference in core scar detection between regular resolution (1.4–2.0 × 1.4–2.0 × 5.0 mm) and 3D high spatial resolution (1.4 × 1.4 × 1.4 mm) late gadolinium enhancement (LGE)-CMR, but more accurate characterisation of the border zone scar region using high spatial resolution CMR with thresholds set at 40–60% of maximal signal intensity (SI).22 The border zone scar region on 3D LGE-CMR correlated with scar on EAVM in 79.2% of patients, compared with only 37.7–61.8% with 2D regular resolution CMR. However, there were only seven NICM patients in this 30-patient cohort referred for VT ablation.22
The feasibility of delineating small VT isthmuses on LGE-CMR in NICM requires further investigation. Siontis et al. compared acute and long-term ablation outcomes in idiopathic dilated cardiomyopathy (IDCM) patients with and without pre-procedural LGE-CMR and found that patients in whom pre-procedural LGE-CMR was performed and areas of possible VT substrate were defined, had higher acute procedural success (63% versus 24%; OR 7.86; p<0.001) and improved survival free of the composite endpoint of VT recurrence, heart transplantation or death (27% versus 60%; p=0.02).23
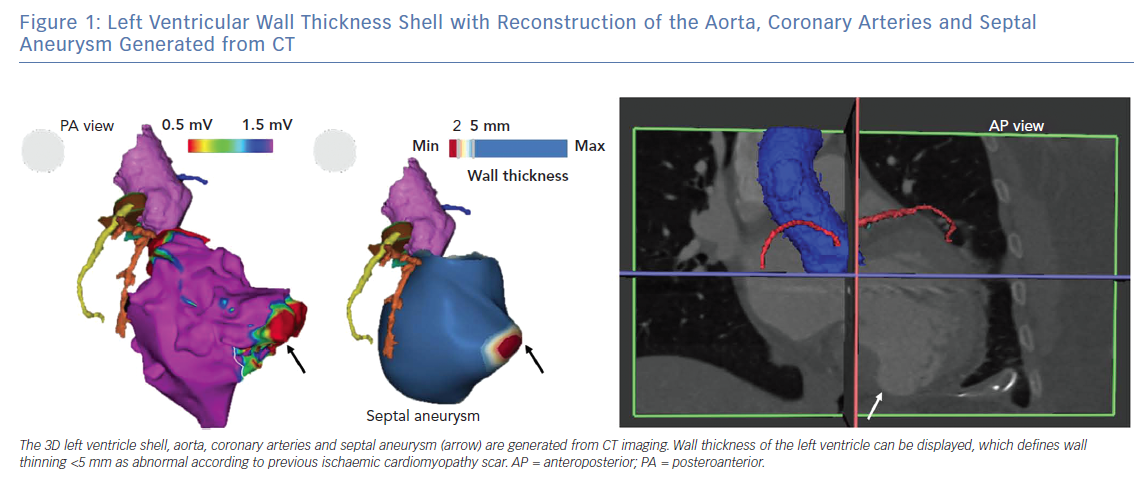
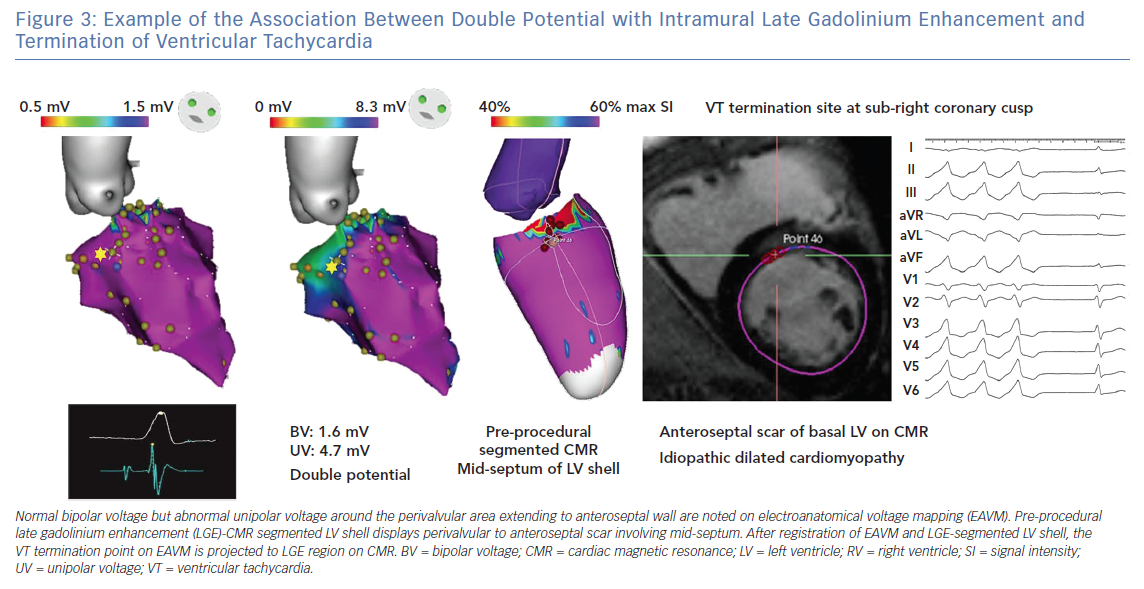
Cardiac CT imaging is another helpful imaging modality to guide NICM VT ablation. Esposito et al. identified arrhythmogenic substrate in 39 of 42 patients utilising CT with delayed enhancement.24 Piers et al. integrated CT and LGE-CMR images simultaneously in 10 NICM patients and proposed an algorithm to detect epicardial and intramural arrhythmogenic substrate.25 They found that in areas with fat thickness >2.8 mm, bipolar or unipolar voltage were attenuated and electrogram duration was lengthened, leading to failure of scar delineation from normal myocardium. In contrast, abnormal electrogram morphologies (late potentials, double potential, fragmented or >4 sharp spikes) could identify the substrate even with the existence of thick fat. In their study, a unipolar voltage cut-off value ≤7.95 mV was able to detect intramural scar. In a study by Yamashita et al., in which image-integration was used to guide VT ablation in 116 patients, 89% of critical VT isthmuses and 85% of local abnormal ventricular activities (LAVA) sites could be identified.21 The efficiency in identifying LAVA with imaging was higher in ICM (90%) and ARVC (90%) than in NICM (72%).
Figure 1 shows an LV wall thickness shell with reconstruction of the aorta, coronary arteries and septal aneurysm generated from CT. Figure 2 shows a pre-procedural LGE-CMR image depicting anteroseptal patchy scar and inferolateral transmural scar. Registration of the CMR-segmented LV shell to endocardial and epicardial EAVM by using landmarks of aorta, LV apex and mitral annulus is successfully accomplished.
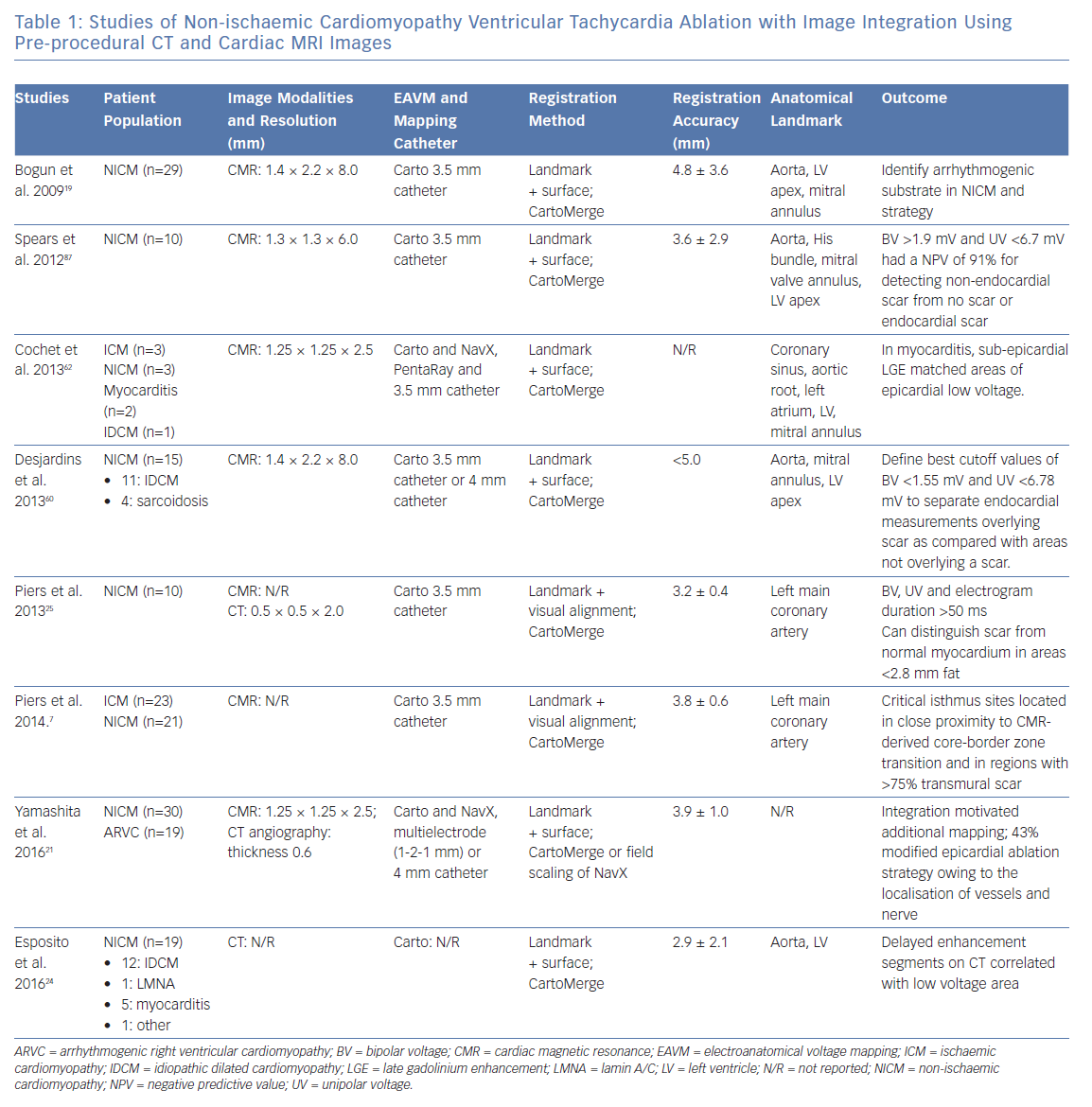
Pre-procedural images can be segmented and displayed as 3D shells and integrated into the electroanatomical map for intraprocedural use. Since critical VT circuits can be quite small, accurate registration of the CT or CMR-segmented 3D models with the EAVMs is crucial to permit precise evaluation of structural as well as electrical abnormalities. Utilisation of intracardiac echo for identification of the cusps and true LV/right ventricle (RV) apices, and their use as landmarks can be extremely helpful for accurate image registration at the time of the procedure. The landmarks and registration distances between CMR or CT-segmented images and electroanatomical maps as well as their impact on outcome in different studies are summarised in Table 1.
VT Substrate Patterns in Different Non-ischaemic Cardiomyopathy Aetiologies
Idiopathic Dilated Cardiomyopathy
There are two predominant substrate patterns in patients with IDCM as identified by unipolar voltage on EAVM and LGE-CMR.26–28 the first is a basal, anteroseptal scar pattern, which frequently extends to the perivalvular region, as well as subepicardial, and the second is an inferolateral or true posterior scar pattern. Identifying the scar pattern in IDCM with pre-procedural imaging allows one to anticipate acute and long-term ablation success, and provide valuable information to share with patients prior to their procedure.
While acute ablation success rates are similar between these two scar patterns, patients with anteroseptal as opposed to inferolateral scar pattern are more likely to have long-term VT recurrence and require repeat ablation.27 In addition, the anteroseptal scar pattern often predicts VT circuit location near the conduction system, prompting pre-procedural discussion about the possibility of atrioventricular block and need for permanent pacing strategies. Frequently, anteroseptal scar patterns extend to involve extensive areas of the endocardial and epicardial perivalvular LV.
Oloriz et al. have previously characterised electrogram abnormalities correlating with CMR substrate and reported that late potentials were more frequently seen on the epicardium in patients with an inferolateral (80%) versus anteroseptal (7%) scar pattern.27 Differences in ablation success between these two groups are likely to be a result of difficulties in targeting VT substrate in the anteroseptal group, as well as the higher prevalence of septal hypertrophy. While patients with inferolateral substrate are more likely to have epicardial late potentials that may be amenable to ablation from the epicardium or coronary venous system, those with anteroseptal substrate frequently have deep intramyocardial substrate within the interventricular septum or LV summit, where effective energy delivery and substrate elimination is difficult with currently available tools.
Our group have also reported a strong association between electrogram characteristics and the transmural extent and intramural types (endocardial, mid-wall, epicardial, patchytransmural) of scar as measured on LGE-CMR in IDCM. Myocardial wall thickness, scar transmurality, and intramural scar types were independently associated with electrogram amplitude, duration, and deflections. Fractionated and isolated potentials were more likely to be observed in regions with higher scar transmurality (p<0.0001 by ANOVA) and in regions with patchy scar (versus endocardial, mid-wall, epicardial scar; p<0.05 by ANOVA). Most VT circuit sites were located in scar with >25% scar transmurality.18
Figure 3 shows a patient with NICM in whom VT was terminated with ablation at a site from LV endocardium that correlated with intramural scar identified by low unipolar voltage of EAVM and LGE-CMR.
In addition to LGE-CMR, fludeoxyglucose (FDG)-PET imaging holds promise for dissecting the role of active inflammation in NICM VT patients.
Tung et al. showed that nearly half of patients referred with unexplained cardiomyopathy and ventricular arrhythmia have focal myocardial inflammation on PET, suggesting an occult arrhythmogenic inflammatory cardiomyopathy in these ‘idiopathic’ NICM patients.29 The potential benefit of immunosuppressive medical therapy is unclear. One review suggested that identification of arrhythmogenic inflammatory cardiomyopathy, may prompt the usage of the anti-inflammatory medical therapy in early stage of arrhythmia before catheter ablation.30 Further efforts on establishing optimal diagnostic and treatment paradigms for NICM VT and premature ventricular contraction patients are warranted.
Cardiac Sarcoidosis
Cardiac sarcoidosis (CS) is an under-diagnosed aetiology of NICM. Cardiac imaging modalities, including LGE-CMR and PET, have dramatically improved the diagnosis of CS and can define the substrate in patients undergoing VT ablation.31–33 The distribution of LGE in patients with CS is variable and frequently patchy, often involving the interventricular septum (predominantly involving the basal and/or mid-ventricular septum, with or without RV involvement) and inferolateral wall.34,35 Additionally, LGE is more frequently seen in subepicardial layers.36
Muser et al. reported that approximately one-third of all affected cardiac segments revealed transmural LGE with preserved wall thickness in patients with CS and VT undergoing ablation.37 The presence of LGE on CMR identifies areas with inflammation, granuloma and scar on necropsy.38,39
Interestingly, compared to patients with IDCM, those with CS tend to have more abnormal electrograms.37 Whether fibrosis or active inflammation represents the main culprit contributing to sustained monomorphic VT remains unclear.37,40,41 Blankstein et al. demonstrated that the presence of focal perfusion defects with 82rubidium nuclear scanning and FDG uptake on cardiac PET identified patients at higher risk of VT or death.40 In contrast, Muser et al. found that the abnormal electrograms were more correlated with LGE on CMR rather than inflammation identified by PET.37 Figure 4 shows an example of fractionated electrograms located in the LGE region on CMR, with good pace-mapping QRS morphology similar to clinical VT morphology.
While there is no definite benefit of immunosuppressive therapy in patients with monomorphic VT and NICM, this strategy is a reasonable approach in patients with CS and VT, particularly in the acute inflammatory phase of the disease when polymorphic VT may be manifest. VT characteristics and ablation outcomes can differ based on the degree of active inflammation with CS, and VT ablation outcomes in patients with CS tends to be worse than other aetiologies of NICM.1,5,42
Lamin A/C Cardiomyopathy
LMNA cardiomyopathy can present in a similar manner to CS, with conduction abnormalities, ventricular arrhythmias and heart failure. The diagnosis can be confirmed with advanced genetic testing.
Consideration of the diagnosis of LMNA cardiomyopathy should be made in all patients with suspected CS who do not respond to anti-inflammatory treatment or who do not have evidence of active inflammation on PET imaging. The specific substrate pattern in LMNA cardiomyopathy, as characterised by CMR, predominantly involves the basal and anteroseptal segments with preserved wall thickness.
Importantly, VT ablation outcomes in patients with LMNA cardiomyopathy tend to be among the worst of all NICM subgroups.43,44
One study reported a dismal 25% success rate despite multiple ablations, and frequently requiring supplementary techniques such as ethanol injection or surgical ablation. Furthermore, nearly all (91%) patients had ≥1 VT recurrence after the last procedure, and the disease process tended to rapidly progress, with a mortality rate of 26% of patients, and a high rate of heart transplantation because of end-stage heart failure.44 Reasons for poor success with VT ablation in patients with LMNA cardiomyopathy include poor accessibility of the substrate which tends to be basal septal and intramural.
Myocarditis
Myocarditis is an important cause of dilated cardiomyopathy worldwide. LGE-CMR and T2-weighted sequences are useful imaging methods for diagnosis of myocarditis.45 The pattern of VT substrate in patients with post myocarditis cardiomyopathy typically involves the sub-epicardium and lateral basal LV, and a combined endocardial and epicardial approach is frequently necessary to achieve durable VT elimination.46,47 A recent multicentre study of 50 patients with myocarditis-related VT reported 1-year VT recurrence rate of 23%.5
Left Ventricular Non-compaction
LVNC is a rare genetic cardiomyopathy, which results from the cessation of embryogenesis of endocardium and mesocardium, generating two-layered structure of the myocardium with a compacted, thin epicardial layer and a non-compacted, thickened endocardial layer with deep intertrabecular recesses. This process mostly affects the inferior and lateral wall from mid to apical LV.48–51 Muser et al. showed that areas with abnormal electroanatomical substrates and low bipolar voltage in patients with VT and LVNC correlate well with non-compacted segments seen on CMR or echocardiography in the majority (75%) of patients.52 Wan et al. found that LGE was detected on CMR in 19 of 57 patients with LVNC, with variable distribution and frequently involving the septum.53 The mechanisms by which LGE develops in patients with LVNC are not understood.
Arrhythmogenic Right Ventricular Cardiomyopathy
ARVC is an inherited cardiomyopathy, which is characterised by cardiac myocyte degeneration and fibro-fatty replacement. Akdis et al. suggested that typical ARVC is the right-dominant subtype of arrhythmogenic cardiomyopathy, which is predominantly associated with mutations in genes encoding proteins of the intercalated disc.54 The other two subtypes, including biventricular form and left-dominant form, are mimics of other NICM including sarcoidosis. ARVC can also occur without evidence of desmosomal protein abnormalities suggesting a predominant role for a triggering mechanism and not a genetically determined degenerative disease.
The exact triggering mechanism for disease manifestation and progression is poorly understood but the absence of rapid scar progression appears to be the rule rather than the exception.55 Fibro-fatty tissue infiltration typically extends from the epicardial surface or mid-myocardium, and may involve the entire thickness of the myocardium.56 CT can identify arrhythmogenic substrate for ARVC patients. Komatsu et al. demonstrated that the majority of LAVAs were located in segments with extensive intramyocardial fat (80%).57 Yamashita et al. also demonstrated a 90% agreement between LAVAs and hypo-attenuated areas identified on multi-detector CT.21
Correlation Between Substrate Derived with Electroanatomical Voltage Mapping and Cardiac MRI/CT/PET
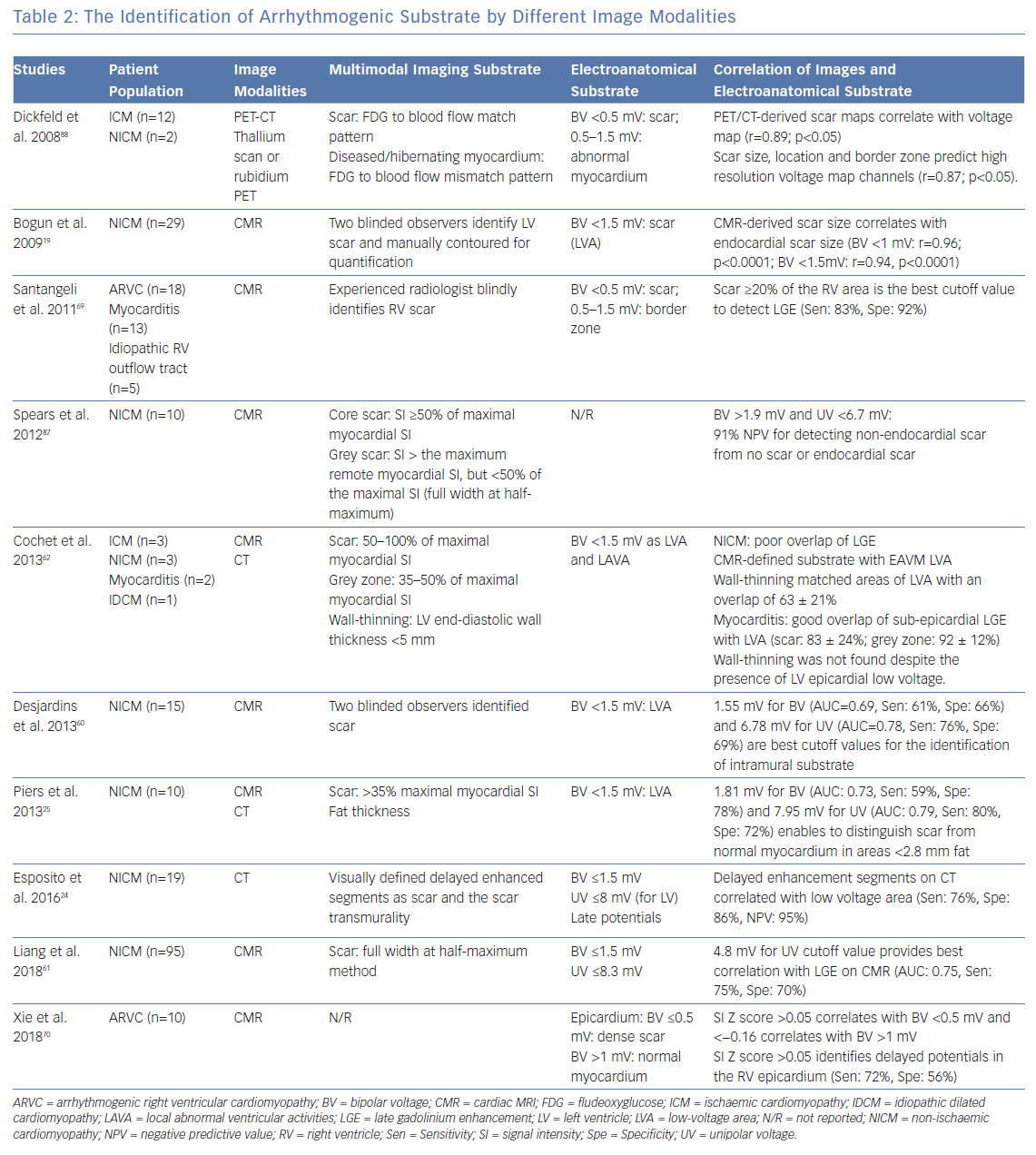
Prior electroanatomical voltage mapping studies have defined normal endocardial and epicardial bipolar voltage cut-offs of >1.5 mV and >1 mV, respectively, and normal unipolar voltage cutoff of >8.3 mV.58,59
Different voltage cut-off values have been proposed to identify scar based on correlation with multimodality imaging. Desjardins et al. evaluated 11 IDCM and four sarcoidosis patients with intramural scar detected on LGE-CMR utilising full width at half maximum (FWHM) method, and identified bipolar and unipolar voltage cut-offs of 1.55 mV and 6.78 mV, respectively, to define intramural scar.60
Meanwhile, Liang, et al. identified a unipolar voltage cut-off of 4.8 mV to best correlate with interventricular septal scar defined by FWHM on CMRI in patients with IDCM and VT but noted that VT electrogram substrate and origin of VT can occur in approximately 10–20% of patients in the absence of LGE in regions with low unipolar voltage using the higher cut-off value of 8.3 mV.61
In a series that included 15 patients (10 with IDCM and five with CS), we determined that voltage thresholds of 1.78 mV and 5.64 mV for bipolar and unipolar scar, respectively, maximise both sensitivity and specificity for identification of LGE on CMR.18 Piers, et al. identified LV endocardial bipolar and unipolar voltage cut-offs of 2.04 mV and 9.84 mV to define scar correlating with LGE-CMR (modified FWHM, ternary method set SI thresholds at 35% and 50% of maximal SI).28 During epicardial voltage mapping, Piers et al. identified bipolar and unipolar voltage cut-offs of 1.81 mV and 7.95 mV, respectively, to correlate with LGE-CMR in 10 NICM patients with VT.25
Maccabelli et al. showed that 95% of patients with myocarditis-related VT had subepicardial LGE on CMR that correlated with areas of unipolar voltage <8 mV.46 Of note, the above-mentioned studies utilised a 3.5 mm tip open-irrigated catheter with 2 mm ring electrode and 1 mm inter-electrode spacing, or a solid-tip 4 mm catheter for EAVM sampling. Importantly, the validity of different voltage cut-off values for defining abnormal substrate should be confirmed/established for maps created using catheters with different interelectrode spacing and specifically when using small electrode size recording tools.
The utility of CT imaging to define VT substrate in patients with NICM has been less well defined. In a small study of 12 patients with IDCM, Esposito et al. demonstrated good correlation between CT-defined substrate (wall thinning <5 mm on CT angiography or visually defined enhanced segments on delayed-enhanced CT) with areas of bipolar and unipolar scar detected with EAVM.24
Cochet et al. acquired high-density endocardial and epicardial EAVM and registered to CMR/multi-detector CT, and found that LGE on CMR and wall-thinning <5 mm at CT corresponded to low voltage areas with bipolar voltage <1.5 mV and LAVA.62 On the contrary, Yamashita et al. demonstrated a poor correlation between wall thinning and EAVM scar (13 ± 16% agreement) in 28 NICM patients with multi-detector CT imaging.21
To date, no studies have investigated the correlation between the substrate on EAVM and LGE on CMR or delayed perfusion area on CT in hypertrophic cardiomyopathy patients, and the effect of ventricular hypertrophy on scar voltage cut-offs with EAVM remains unclear. Bazan et al. demonstrated that the myocardial wall thickness or distance from the normal tissue to the abnormal substrate is one of the key factors that can influence the interpretation of abnormal unipolar voltage cut-off value.63 In patients with hypertrophy, the applicable unipolar cut-off value when using a 3.5 mm electrode tip may be greater than the standard 8.3 mV cut-off.64,65
Titrating the slider bar up to 10 mV, or even higher, in the setting of LV hypertrophy may permit identification of areas with layered mid-myocardial or epicardial scar. Glashan et al. confirmed the linear association of wall thickness with both unipolar or bipolar voltage in the myocardium without fibrosis detected by histology.66 In these scenarios, certain regions that ‘ghost in’ when adjusting the slider bar upwards may represent areas of intramural and epicardial substrate in patients with LV hypertrophy.
Several important issues must be considered when evaluating RV substrate. First, the RV free wall is thin and normal voltage cut-offs differ from the RV septum. Second, the aortic root, which overlaps the RV septum to RV outflow tract (RVOT), can influence the normal voltage cut-off. Finally, in addition to scar, fat can be arrhythmogenic in patients with ARVC.
Normal RV endocardial voltage cut-offs, based on studies examining patients with normal ventricles without evidence of EAVM or CMRI scar, have been identified to be >1.5 mV (bipolar) and >5.5 mV (unipolar, free wall).58,64,67 However, we have shown that unipolar voltage correlating with CMR scar along the posterior RVOT opposite the aortic root tends to be lower than the rest of the posterior septal area, and the authors calculated optimal unipolar voltage cut-off values of 6 mV for the posterior aspect of the RVOT opposite to the aortic root and 7.5 mV for the remainder of the septal aspect of the RV.68
Santangeli et al. reported in a mixed cohort of 18 patients with ARVC, 13 patients with myocarditis and five with idiopathic RVOT arrhythmias that the distribution of LGE correlated well with the distribution of EAVM scar defined as bipolar voltage of <1.5 mV, including free wall, posterior/inferior wall as well as RVOT. However, the existence of LGE on CMR missed 91% of EAVM substrates when the RV EAVM scar area was <20%, indicating that EAVM is much more sensitive for substrate identification than CMRI when the scar burden is low.69
Recently, we reported the association of regional LGE-CMR standardised intensity with 3,205 epicardial electrogram map points in 10 ARVC patients. Bipolar (−1.43 mV/z-score; p<0.001) and unipolar voltage amplitude (−1.22 mV/z-score; p<0.001) were associated with regional signal intensity standardised by z-scores. Signal intensity z-score thresholds >0.05 (95% CI [−0.05–0.15]) and <−0.16 (95% CI [−0.26–0.06]) corresponded to bipolar voltage measures <0.5 and >1.0 mV, respectively.70 The characterisation of different image modalities in association with arrhythmogenic substrates are summarised in Table 2.
Innovative Image-guided Treatments
Recently, innovative imaging-guided treatments have been utilised for refractory VT patients. For patients with severe adhesions post cardiac surgery or repeated epicardial ablations limiting standard percutaneous epicardial access, Aksu et al. described a minimally invasive surgical approach to achieve epicardial access via video-assisted thoracoscopy.71 Stereotactic body radiation therapy (SBRT) is an increasingly utilised non-invasive therapy for patients with refractory VT.
Cuculich et al. performed SBRT in five high-risk refractory VT patients and demonstrated dramatic reduction of VT burden over long-term follow-up.72 The recent Phase I/II Study of EP-guided Noninvasive Cardiac Radioablation for Treatment of Ventricular Tachycardia (ENCORE-VT), was a single-arm prospective study that demonstrated SBRT to be associated with marked reduction of VT burden, and as such may be a viable alternative treatment option for patients with VT refractory to ablation.73
Sympathetic hyperactivity clearly plays a vital role in the genesis and maintenance of ventricular arrhythmias, and cardiac sympathetic denervation has been reported as the effective VT treatment which can reduce the burden of ICD shocks.74-76 Vaseghi et al. demonstrated that bilateral cardiac sympathetic denervation is more beneficial than left cardiac sympathetic denervation in VT storm patients.77 Of note, PET imaging can be helpful in assessing cardiac sympathetic innervation.78
Limitations of Cardiac Imaging Assessment and Image Integration
Image Resolution and Presence of ICDs
It is challenging to delineate the border zone substrate using partial volume averaging with LGE. Schelbert et al. acquired CMR imaging utilising 7 Telsa scanner to identify post-infarction myocardial fibrosis in the ex vivo rat heart and demonstrated that the intermediate signal intensity is resolution dependent.79 Of note, high resolution images can identify intermediate signal intensity voxels correlating with histological fibrosis and a possible VT isthmus, but blur with normal myocardium when image resolution declines due to partial volume effect.
In patients with pacemakers and ICDs, imaging artifact from the pulse generator and leads can limit the interpretation of substrate from CMR or CT. The application of a wideband LGE sequence has reduced the hyper-enhanced CMR artifact, however, the dark magnetic susceptibility artifacts remain problematic. Additionally, the current 3D in-plane resolution of wideband sequences is limited to 1.5 × 1.5 mm with slice thicknesses ranging from 4–8 mm, which may not be sufficient to clearly delineate critical VT isthmuses.80,81 One advantage of CT compared with delayed enhancement (DE)-CMR is that device-related artifact can be quantified logically: each voxel with a value >20% of the maximum density can be considered as hyperdense artifacts, while voxels with values less than −150 HU can be considered as hypodense artifacts.82
Furthermore, although evolving evidence indicates that CMR can be safely performed in patients with devices, including those who are pacemaker dependent, and even in those with abandoned leads or non-MRI conditional systems,CMR may not be universally offered by all centres for patients with ICDs at the current time.83,84
Functional Ventricular Tachycardia Isthmus Assessment
The above-mentioned imaging modalities focus on the detection of structural abnormalities and their association with demonstrated EAVM substrates in non-ischaemic VT patients. Few studies have correlated the imaging detected abnormalities to the functional VT isthmuses in NICM patients.7
Anter et al. identified the VT critical isthmus zone, corresponding to the location of a steep activation gradient and very low voltage amplitude during sinus rhythm in the post-infarction swine model.85 The functional electroanatomical high-density mapping allows identification of VT reentrant circuits whilst the EAVM or electrograms during sinus rhythm have limited specificity to identify VT circuits.
Ciaccio et al. proposed the source-sink mismatch model to explain how the ischaemic VT re-entrant circuits form and become sustained.86 Of note, it is typically challenging to precisely identify non-ischaemic VT circuits and correlate circuit components with imaging structural abnormalities due to the haemodynamic instability and multiple VT morphologies.
Lack of Evidence Associating Histology and Non-ischaemic Scar Detected by Cardiac MRI or CT
There is no agreement on the optimal method and SI thresholds, as well as CT attenuation thresholds to delineate fibrosis/scar or border zone area within scars validated by histology in the setting of prior infarction. Prior studies have utilised various methods to identify fibrosis/scar on the LGE-CMR and CT angiography. By LGE-CMR, the thresholds can be defined using standardised myocardial SI.
One methodology sets thresholds at 35%, 50% or 40% and 60%7,28,22 to distinguish scar core and border zone area from normal myocardium. For NICM patients, 6 standard deviations above the average SI of healthy remote myocardium has been utilised to define scar.18 In CT, scar may be estimated as hypo-attenuation regions on immediate first pass imaging, or as hyper-attenuation regions on DE imaging acquired 10 minutes after contrast agent injection.
Similar to CMR, the extent of scar based upon CT attenuation can be assessed visually or quantitatively using specialised software. Wall thinning <5 mm with LV bulging or aneurysmal dilation can also be used to estimate scar distribution.24 Compared to CMR, CT offers exceptional spatial resolution. However, CMR offers improved temporal and contrast resolution. The optimal method to identify scar employing either LGE-CMR or CT imaging remains to be definitively elucidated and will likely depend upon the patient condition, renal function, ability to breath hold, and institutional resources. The current evidence for scar delineation by imaging in NICM is primarily based on the association with electroanatomical mapping and abnormal electrograms.
Conclusion
The underlying VT substrate in patients with NICM can be quite variable, depending on the underlying NICM aetiology. Pre-procedural multimodality imaging and intra-procedural image integration can be helpful to delineate VT substrate and facilitate safe and effective VT ablation in patients with NICM.
Clinical Perspective
- The arrhythmogenic substrate can differ, depending on the aetiology of non-ischaemic cardiomyopathy (NICM).
- Multimodality imaging is helpful to characterise the substrate in patients with NICM prior to ventricular tachycardia
(VT) ablation. - Image integration, although not yet characterising detailed histology, can delineate the location and extent of the VT substrate and appears to facilitate safe and effective VT ablation.