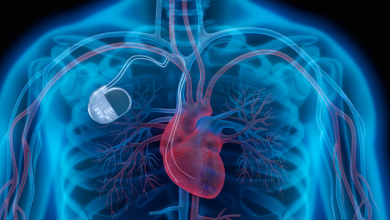
Electrophysiology has rapidly transformed from diagnostic cardiac studies to direct therapeutic interventions. Many cardiac arrhythmias that formerly required the use of drugs or surgery can now be routinely cured in the electrophysiology laboratory by means of transcatheter ablation techniques.
Arrhythmia
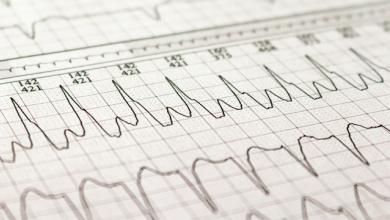
Arrhythmia, or ‘an irregular heartbeat’, is a fairly common condition in which the patient suffers from an abnormal heart rhythm. Heart arrhythmias occur when the electrical signals responsible for coordinating the heart’s beats don’t work properly, resulting in a heart that beats too fast, too slow or irregularly.
Symptoms of heart arrhythmia may include the following:
- An abnormally fast heartbeat
- An abnormally slow heartbeat
- Chest pain
- Shortness of breath
- A fluttering feeling in the chest
- Heart palpitations
- Dizziness
- Fainting
- Anxiety
Heart arrhythmias fall into several different categories. Below are the different types of heart arrhythmia:
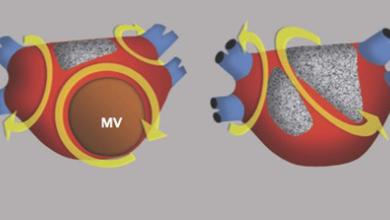
- Atrial fibrillation - The most common type of heart arrhythmia, with the heart beating irregularly and faster than normal.
- Supraventricular tachycardia - The heart will suddenly start beating much faster than normal, sometimes for a few minutes but it can last hours.
- Bradycardia - The heart beats slower than normal, less than 60 times per minute.
- Heart block - Also known as AV block, this is when the electrical signals controlling your heart beat become blocked, resulting in a slower or irregular heartbeat as it struggles to pump blood effectively.
- Ventricular fibrillation - This is an incredibly dangerous type of arrhythmia where rapid and chaotic electrical signals cause the heart’s ventricles to quiver (fibrillate) preventing blood from being pumped around your body.
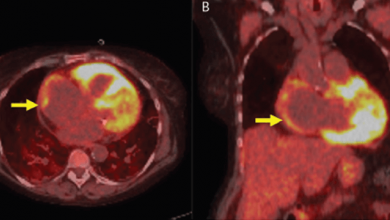
In order to diagnose the type of arrhythmia the patient is suffering from, an electrophysiology (EP) test may be conducted.
What is electrophysiology?
Electrophysiology is the study of the electrical properties of biological cells. As it relates to arrhythmia, an electrophysiology (EP) study, sometimes called ‘invasive cardiac electrophysiology’, is a series of tests that examine the heart’s electrical activity, therefore enabling cardiologists to diagnose any potential heart problems.
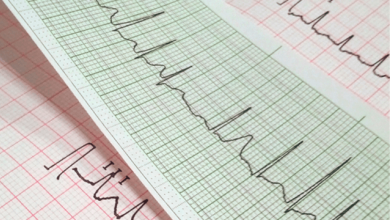
Clinical electrophysiological techniques have evolved for the assessment of sinus nodal, AV nodal and His-Purkinje system function. The evaluation of tachyarrhythmias has progressed rapidly, and pharmacological, device and surgical therapy can now be guided by electrophysiology of heart and arrhythmias studies.
Electrophysiology of heart and arrhythmias
For patients that have suspected heart arrhythmia or other heart related issues, electrophysiology can help to identify and diagnose the issue in order to prescribe appropriate treatment. Below outlines the basic electrophysiology study process:
- Often, a few days before an EP study, blood tests and an electrocardiogram (ECG) test will be conducted first to record the electrical activity of the heart.
- The patient will have to fast for 6 - 8 hours before the procedure. Just before the EP study, the patient will be asked to empty their bladder.
- An IV line is started in the hand or arm and a sedative is often administered to help the patient relax.
- Electrodes and a blood pressure cuff are often attached to the patient for monitoring purposes.
- Local anaesthetic is injected at the site where the catheters, or wire electrodes, are inserted. Thin wire electrodes are then inserted into a vein in the groin or neck and are threaded through to the heart. A fluoroscopy is used to guide the wire electrodes.
- Small electrical impulses are then sent to the heart to measure its reaction.
- The catheters are then removed and the results of the study analysed.
Supraventricular arrhythmias can exacerbate the heart failure symptoms by decreasing the effective cardiac output and control requires pharmacological, electrical or catheter-based intervention.
In patients with atrial flutter or atrial fibrillation, anticoagulation is paramount to prevent systemic or cerebral embolism. People with heart failure are also prone to develop ventricular arrhythmias that can present a challenge to the clinician. The management strategy depends on the type of arrhythmia, the underlying structural heart disease and the severity of heart failure.